Introducing Allergens to Baby

In 2015, a groundbreaking study demonstrated that the early introduction of peanuts to at-risk babies could reduce the risk of developing peanut allergy by as much as 81%. In other words, delaying the introduction of peanut could actually increase the likelihood of peanut allergies developing.
This landmark study led medical authorities to revise their recommendations around the introduction of peanut and extrapolate the findings to other food allergens as well. As such, allergists and medical institutions now recommend introducing many common food allergens before a baby’s first birthday.
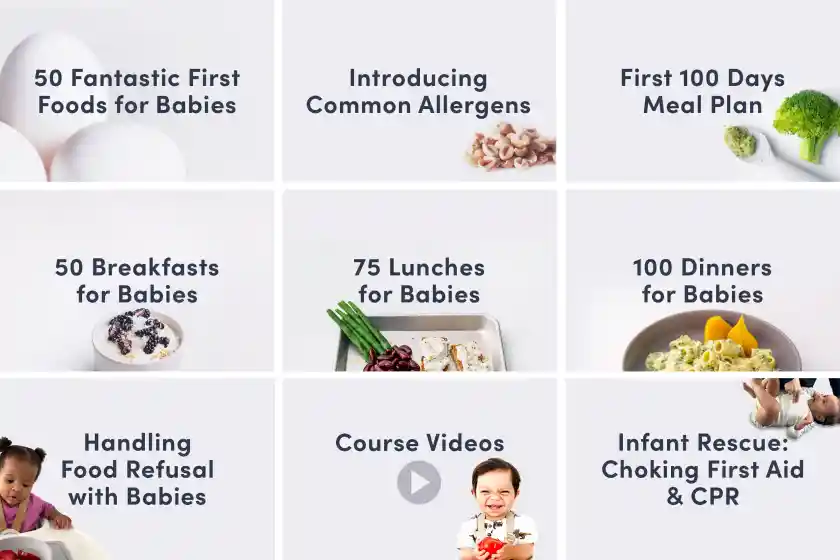
Just starting solids? See our First 100 Day Guide, our Introducing Allergens Guide, or browse our full collection of guides for starting solids with babies.
Allergies in children are on the rise
In the United States, food allergies in children rose an astounding 50% from 1997 to 2011 and the prevalence of peanut and tree nut allergies tripled during this time. Interestingly, this is roughly the same period of time in which parents were advised to refrain from introducing peanuts and other allergens until well beyond a child’s first birthday. With the new guidelines to introduce allergens early, our hope is that the number of babies and children with allergies will start to decline.
Common food allergens for babies
Today, one in 13 children have a food allergy in the U.S., with cow’s milk and hen’s egg the most common allergies for babies. Of those children with food allergies, 40% will be allergic to more than one food.
Although it is possible to be allergic to any food, the most common food allergens are those listed below. Sesame allergies are on the rise, and because of a law enacted in 2021, products containing sesame will be required to be labeled in the United States starting in 2023.
Finned Fish
Shellfish
Soy
Tree Nuts
Is my baby at risk for food allergies?
Before introducing major food allergens, it’s important to know if your baby is at an increased risk of developing food allergies. Interestingly, there are only a couple of conditions that would prompt allergists to potentially take a more cautious approach to food allergen introduction.
A food allergy can develop at any point in a person’s life, but there are risk factors that you can identify early on:
Severe eczema. Eczema is a common childhood rash caused by a defect in the skin barrier and tends to present as dry, inflamed, and intensely itchy patches on the skin. Eczema is thought to increase the chances of becoming sensitized to a food allergen through the compromised skin barrier. Severe eczema, in particular, is widely considered a significant risk factor for developing food allergies. Although there is no formalized international definition of severe eczema, most physicians consider eczema severe if it covers a large percentage of body surface area or persists for an extended period of time despite the regular application of moisturizers and topical anti-inflammatory medications. Note: Although mild-moderate eczema is associated with a small increase in the risk of developing food allergy, well-controlled eczema of lower severity does not warrant any change in the approach to allergen introduction compared to children who do not have eczema.
Existing food allergies. While not as much of a risk factor as severe eczema, if your baby has an IgE-mediated allergy to one food, they may have a higher risk of developing another food allergy. For example, babies with existing egg or milk allergies are known to be at an increased risk of developing peanut allergy. Note: Although there is not enough data to definitively state that existing allergy to other common food allergens (such as tree nuts, wheat, soy, or seafood) is also associated with an increased risk of developing additional food allergies, allergists will often take a proactive approach to introducing food allergens for these babies.
If your baby has either of the above risk factors, work closely with your pediatrician, family doctor, or pediatric allergist early in your solid food journey. They can help you map out a plan to safely introduce potential food allergens into baby’s diet, order allergy testing, or supervise allergen introduction in the clinic. Otherwise, aim to introduce the common food allergens between 6 and 12 months of age, and regularly maintain them in the diet after introduction.
What about family history of allergy?
Although it was previously believed that a family history of food allergies might predispose a baby to food allergy, there is no evidence that a younger sibling of a peanut-allergic child, for example, is at increased risk of developing peanut allergy. Allergy specialists now recommend that siblings of children with food allergies can introduce common food allergens in the home without any pre-screening by an allergist if they are not at higher risk due to severe eczema or another pre-existing food allergy.
Studies suggest that the deliberate delay of food allergen introduction in siblings of allergic children may put the younger sibling at increased risk of developing a food allergy. Essentially, the risk of delayed introduction is higher than the risk posed by family history. Nevertheless, if the idea of a home-based introduction is anxiety-provoking due to family history, you may be able to request allergen introduction in the clinic, under medical supervision.
How to introduce allergenic foods to babies
Introducing food allergens doesn’t have to be terrifying. You can start with a very small amount of the allergen to minimize any possible reaction and slowly work up to larger servings. If you are anxious to introduce allergens to your baby, consider following our First 100 Days Meal Plan, which provides suggested measurements of each allergen per week and gradually introduces most of the common allergens.
Tips for introducing common food allergens to babies
Start small The smaller the quantity served, the less severe an allergic reaction may be. Start with small amounts, such as 1/8 teaspoon of a finely ground nut added to your baby’s bowl of oatmeal. If there is no reaction, try gradually increasing the amount over the next few days until you work up to larger amounts. Once you’ve ruled out an allergy to that food, aim to offer it to your baby as frequently as possible, but weekly at a minimum.
Introduce allergens early in the day. Most allergic reactions occur within two hours of ingestion and often within minutes. Consider introducing an allergen shortly after waking in the morning or right after a morning nap. Introducing the allergen in the morning lets you observe your child during the day ahead; should an allergic reaction occur, it is easier to contact your doctor for guidance. For similar reasons, it is best to introduce allergens at home and when at least one adult can focus their full attention on the baby (without distraction from other children or household activities) for at least two hours afterward.
One at a time. Introduce one food allergen at a time. This way, if there is a reaction, you’ll know which food was responsible. Not all babies with allergies will react on the first exposure, so it’s important to keep serving sizes small until you are confident there is no allergic reaction. A few days of daily ingestion is enough to establish that a food is well tolerated, but this doesn’t mean you can only offer one new food every few days. Don’t be afraid to offer multiple new foods each week, as long as you aren’t introducing common food allergens simultaneously. Pick a pace that feels comfortable and enables you to introduce a wide variety of new foods well before your baby’s first birthday. Need help or ideas for introducing allergens and a variety of foods? Check out the First 100 Days Meal Plan for Starting Solids
Regular exposure. Once you’ve safely introduced a food allergen to your child, keep that food in regular rotation—consistency is key. Allergists often recommend aiming for the inclusion of common allergens 2-3 times per week because that was the median frequency of allergen exposure reported in major studies on food allergy prevention. However, don’t stress if you can’t get each common allergen on the menu that frequently, and don’t worry if your baby doesn’t consume the entire serving of allergen offered that day. Relatively modest quantities of allergen exposure (~2 grams of protein per week) can be effective for allergy prevention, as long as exposure remains consistent; studies show that even once weekly exposure to common food allergens is beneficial.
Anxious for more? See our full guide, Introducing Allergens.
Allergy FAQs
Should I only introduce one food at a time?
There is no evidence to support waiting 3-5 days between introducing new foods. Introducing foods one at a time in a delayed fashion can significantly limit the timely introduction of foods, and potentially increase the risk of food allergy in the future. In general, the benefits of introducing a variety of new foods outweigh the risks of a potential reaction or sensitivity.
However, for common allergens, it’s wise to introduce those on days when no new foods are introduced, so you know which food was responsible in the case of a reaction.
What is an IgE-mediated allergy?
IgE-mediated food allergies are the result of the abnormal production of IgE antibodies. These antibodies are produced in response to specific proteins—and rarely, carbohydrates—within a food. When IgE antibodies attach to their allergens and bind to receptors on mast cells (a type of white blood cell) in the body’s tissues, it triggers the rapid release of multiple chemical mediators—histamines, leukotrienes, heparin, and more. These mediators are responsible for the signs and symptoms of allergic reactions.
IgE-mediated allergies result in symptoms very quickly after ingestion of a food allergen, often within minutes. Because IgE-mediated reactions can result in respiratory distress, low blood pressure, and decreased blood flow to vital organs, they are potentially life-threatening. For this reason, individuals with IgE-mediated food allergy should be prescribed an emergency supply of auto-injectable epinephrine (adrenaline), which is the only medication proven to rapidly reverse the symptoms of a severe allergic reaction.
IgE-mediated allergies are diagnosed by confirming a clinical history of reactivity with a positive blood test or skin prick test at the allergist’s office. Several IgE-mediated food allergies are commonly outgrown in early childhood.
What is a non-IgE-mediated allergy?
Non-IgE-mediated food allergies are immune hypersensitivities that do not involve the production of IgE antibodies and instead involve other parts of the immune system, such as T-lymphocytes (a type of white blood cell).
Non-IgE-mediated food allergies present in various ways, ranging from skin rashes to gastrointestinal symptoms. In general, the symptoms of non-IgE-mediated food allergies take longer to appear than IgE-mediated allergies, presenting hours to days after exposure. There is no standardized testing available for non-IgE-mediated food allergies, so the diagnosis is based on clinical history. The recommended treatment is avoidance of the allergen with reassessment at regular intervals to determine if the allergy has been outgrown. Epinephrine and antihistamines will not treat the symptoms of non-IgE-mediated food allergy. However, in certain cases, anti-nausea and steroids may be used to counteract the inflammatory response.
What is FPIES?
Food Protein-Induced Enterocolitis Syndrome (FPIES) is a relatively uncommon non-IgE-mediated food allergy in children that can be severe and life-threatening. Unlike most food allergy reactions that occur within minutes of contact with a specific food trigger, FPIES allergic reactions occur within hours after consuming a particular food. For this reason, FPIES is sometimes known as a delayed food allergy.
The most common food culprits are:
Cow’s milk products (such as formula)
Soy
Barley
Meats
Poultry
Seafood
Squash
FPIES is extremely rare in exclusively breastfed infants. The classic presentation of FPIES is an infant who recently switched from human/breast milk to formula or started solids and begins vomiting 1-4 hours and experiencing diarrhea 5-10 hours after ingestion of a specific food. Other symptoms include low blood pressure, low body temperature, extreme pallor, repetitive vomiting, and significant dehydration. Thankfully, most cases of FPIES will completely resolve during toddlerhood. Babies with FPIES should be in the care of an allergist/immunologist and are best served by a multidisciplinary team that also includes their general pediatrician or family practitioner, a pediatric gastroenterologist, and a registered dietician.
Rash on baby’s face from tomato and other acidic foods
Acidic foods such as lemons, limes, oranges, and tomatoes often cause a harmless rash on the skin that comes into contact with the juices. The rash, which typically shows up around the mouth and chin, is typically harmless and usually dissipates within minutes once the skin is gently cleansed (pat with a wet washcloth, don’t rub). To help protect the skin from acidic foods you can apply a barrier ointment, such as pure petroleum jelly or a plant-based oil/wax combination emollient, to the face before mealtime.
If I have allergies or Oral Allergy Syndrome, will I pass them on to baby in my human/breast milk?
Fortunately, allergies and OAS are not passed along to baby through human/breast milk. Concerns about potential food allergies should not discourage parents from offering human/breast milk, especially since human/breast milk offers a variety of nutritional and immune-supporting benefits for baby. Avoiding common food allergens to prevent food allergies either during pregnancy or when lactating hasn’t been shown to prevent food allergies and is not recommended.
If I am allergic to a food, how do I introduce that food to baby?
It can be nerve-wracking to feed your baby a food to which you are allergic. Rest assured that you are unlikely to experience a serious allergic reaction from simply being in the vicinity of your allergen or even from handling it. Most patients with food allergies react only upon ingestion. That said, there are steps you can take to minimize your risk of a reaction.
When preparing the food, avoid prolonged skin contact with the allergen. If you cannot wash your hands promptly afterward, wear gloves.
If you have a carpet or rug, make sure you place baby’s high chair over a splat mat or move the high chair to a non-carpeted surface or even consider feeding baby outside. This is also a great time for disposable placemats, plates, and utensils.
When introducing the allergen, offer the allergen at the beginning of the meal and immediately follow up with another food to which neither you nor baby are allergic. This will reduce the allergen content in baby’s saliva.
After mealtime, clean baby’s hands and face thoroughly, wipe down the eating surface and chair, and remove baby’s clothing so it can be washed.
Lastly, model a calm demeanor, even if you are nervous at first; children pick up on the anxiety of the adults around them. As feedings continue successfully, they will get easier and become routine. If you feel very nervous, this is an excellent opportunity for a non-allergic parent, caregiver, relative, or friend to spend quality time with baby.
If baby was diagnosed with cow’s milk allergy, can they consume other dairy products like yogurt and cheese?
It depends. Dairy items such as yogurt and cheese contain the same allergenic proteins as cow’s milk, and can trigger allergic reactions in sensitive babies. However, if baby is not significantly sensitized to casein, the heat-stable protein in milk, they may be able to tolerate fully baked forms of milk, such as in a muffin or cake. Some babies can also tolerate less extensively heated forms of milk, such as in cookies or homemade pancakes. However, this should be discussed with your healthcare professional before attempting it in the home setting.
Buffalo, goat, and sheep milk products are not recommended for babies with cow’s milk allergy due to high rates of cross-reactivity.
If baby has a non-IgE-mediated cow’s milk allergy and requires an alternative formula, your doctor may recommend skipping soy formula and going directly to a hypoallergenic or elemental formula instead, as babies with this type of milk allergy often react to soy as well.
Research shows the majority of children with cow’s milk allergy will outgrow it by age 6, and many babies with milder symptoms of milk protein allergy—which can show up as painless blood in the stool—can successfully reintroduce cow’s milk as early as their first birthday, with the guidance of their doctors.
If a recipe requires milk, what is the best milk substitute for a baby with cow’s milk allergy?
The best options for an infant with cow’s milk allergy include breast/human milk from an individual who is avoiding dairy and soy in their diet, or a hypoallergenic formula as recommended by your healthcare professional.
For toddlers, fortified pea protein or oat milks are also acceptable substitutes. Note: Compared to cow’s milk, pea protein milk tends to be lower in calories, and oat milk is usually lower in protein; for a full comparison of plant-based milks, see our Milk FAQs. If you desire a source of mammalian milk for your toddler, mare’s milk and camel milk have relatively low rates of cross-reactivity with cow’s milk. Be sure to connect with your pediatric healthcare professional, dietitian, or nutritionist to help identify the best substitute for your child’s individual needs.
Note: Lactose-free formula and milk are not appropriate for a child with cow’s milk allergy. In milk allergy, the whey and casein proteins trigger the allergic reaction, and lactose-free milk still contains these natural proteins.
Do I need to buy products like SpoonfulOne?
It is generally not necessary, nor cost-effective, to depend on powders or medicalized processed food products to introduce food allergens or maintain them in the diet long-term. Babies and children should be encouraged to enjoy a wide variety of whole foods with their associated tastes, smells, and textures intact, in alignment with family preferences and cultural feeding practices. Unless you are unable to access whole food allergens consistently or baby has a medical condition that interferes with the ability to eat solids, allergen exposure with real, unprocessed foods is most ideal.
Food Allergies Around the World
The United Nations and World Health Organization have established the Codex Alimentarius (Codex), a set of international food standards, guidelines, and codes of practice designed to ensure the safety of the global food supply.
The Codex requires disclosure of the following food allergens:
Egg
Milk
Fish
Crustaceans
Gluten
Soy
Peanut
Tree nuts
Sulfites (at concentrations 10 mg/kg or more)
These foods comprise more than 90% of food-induced allergic reactions in most areas of the world. However, common food allergens vary worldwide and are influenced by genetics, the foods most consumed in those regions, and cross-reactivity with airborne allergens, among other factors.
Africa
Several African nations, including Egypt, Malawi, Morocco, and South Africa, have common food allergen lists that mirror that of the U.N./WHO Codex.
Recent research suggests that food allergies may be underdiagnosed across the African continent.
Asia
There is no central regulatory body governing food allergy labeling for the Asian continent, and common food allergens vary in different areas.
Common food allergen lists for China, Hong Kong, Singapore, Thailand, and Vietnam are similar to the U.N./WHO Codex.
Common food allergens in Japan and South Korea include allergens outlined in the UN/WHO Codex, as well as buckwheat.
Additionally, South Korea lists chicken, beef, pork, pine nuts, peach, and tomato as common food allergens.
While chickpeas are not designated as a common allergen requiring labeling, chickpea is a significant emerging food allergen in India.
Central America, South America & Caribbean States
CARICOM (an organization of Caribbean states), the Central American Technical Regulation countries, Brazil, Venezuela, Argentina, and Chile recognize the same common allergens as outlined by the UN/WHO Codex.
Additionally, Brazil requires labeling of products containing natural rubber/latex.
Europe
The European Union (EU) recognizes 14 common food allergens/intolerances—gluten-containing cereals, egg, milk, soy, peanut, tree nuts, fish, crustaceans, mollusks, celery, mustard, sesame, lupin, and sulfites.
Non-EU countries in the region that also follow these guidelines include Iceland, Liechtenstein, Norway, Macedonia, Switzerland, United Kingdom (UK), Belarus, Russia, Turkey, and Ukraine.
North America
In the United States, there are currently nine foods required for labeling as major food allergens—milk, eggs, peanuts, tree nuts, fish, sesame, shellfish, soy, and wheat.
Mexico and Canada recognize and require the labeling of allergens as outlined by the UN/WHO Codex.
Canada includes mustard and sesame on its list of top allergens.
Southwest Asia
The Gulf States Organization (GSO) recognizes the following allergens—gluten-containing cereals, egg, milk, soy, peanut, tree nuts, fish, crustaceans, mollusks, celery, mustard, sesame, lupin, and sulfites.
Of note, sesame is a very prevalent allergen in this region, and in Israel, studies have identified sesame as the second most common food allergen in children, after milk.
Southwest Pacific
Australia and New Zealand require labeling for common allergens as outlined by the UN/WHO Codex.
Additionally, Australia and New Zealand identify lupin, sesame, bee pollen, and royal jelly as common allergens.
Note that many common food allergens are also choking hazards (nuts, nut butters, shellfish, etc.), so be sure to learn how to modify these foods to make the consistency age-appropriate and safe for your baby.
Next up: Symptoms of Allergic Reactions
Reviewed by:
V. Kalami, MNSP, RD, CSP
R. Ruiz, MD, FAAP. Board-Certified General Pediatrician & Pediatric Gastroenterologist
S. Bajowala, MD, FAAAAI. Board-Certified Allergist & Immunologist
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
The content offered on SolidStarts.com is for informational purposes only. Solidstarts is not engaged in rendering professional advice, whether medical or otherwise, to individual users or their children or families. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or your medical or health professional, nutritionist, or expert in pediatric feeding and eating. By accessing the content on SolidStarts.com, you acknowledge and agree that you are accepting the responsibility for your child’s health and well-being. In return for providing you with an array of content “baby-led weaning” information, you waive any claims that you or your child may have as a result of utilizing the content on SolidStarts.com.