Milk FAQs for Babies & Toddlers

There’s a lot to know about milk for babies. Read on to find out how much milk to give, when to give it, and more. Just joining us? Check out our guides on Starting Solids and Toddlers at the Table.
Can babies have dairy before age one?
Yes, in the form of solid foods–but the type and preparation matter. Dairy products such as full fat yogurt, low-sodium cheeses, butter, and ghee, are fine to offer to your baby after 6 months of age in age-appropriate amounts after having successfully introduced iron-rich foods (cow’s milk is low in iron). Since cow’s milk as a drink is consumed in greater amounts than the other dairy foods mentioned, it often takes the place of breast milk and formula intake. Its introduction before 11-12 months of age can lead to issues like iron deficiency anemia and intestinal distress, due to the fact that it is nutritionally incomplete, low in iron, and can have difficult-to-digest proteins.
Small amounts of milk can also be used in cooking, as long it doesn’t replace breastmilk or formula intake. This can be confusing since cow’s milk or other milk drinks are not usually recommended until after 12 months of age.
Do babies and toddlers need cow’s milk?
No, though the American Academy of Pediatrics does recommend plain cow’s milk for toddlers 12 months and older as a source of essential fat and nutrients, including calcium, vitamin D, protein, vitamin A, and zinc. That said, if your child is 12 months or older, meeting growth chart standards, without health concerns or allergies that may affect diet and eating a wide variety of fresh foods high in the aforementioned essential nutrients, cow’s milk (or any milk, plant-based or otherwise) may not be necessary. If you want to avoid animal milk entirely, it would be wise to work with your pediatrician and/or pediatric dietitian to ensure your child is receiving optimal nutrients.
When can babies drink cow’s milk?
Most pediatric organizations have recommended waiting until a baby’s first birthday to introduce cow’s milk as a drink as the digestive systems of babies may not tolerate cow milk protein in large quantities well. Compared to breast milk or formula, cow’s milk is nutritionally incomplete, which means that it does not provide all of the healthy fats and nutrients that your baby needs to thrive. While cow’s milk forms the base for most infant formulas, it is modified in formula to make it nutritionally similar to human milk.
Dairy products like yogurt and cheese, however, can be introduced as early as 6 months of age. Because they are fermented, the harder-to-digest proteins can become partially broken down, and may make them easier for baby to tolerate. Ghee and butter have minimal to no protein and are usually well tolerated by babies.
Around 11 months of age, it is our opinion that it’s okay to offer small sips of cow’s milk (about 1 ounce) in an open cup to encourage your baby’s drinking skills and to acclimate your child to the new taste. Just avoid replacing breast milk or formula feeds with cow’s milk. Cow's milk should ideally never be served in a bottle, but it can be offered in an open cup or with a straw. Babies who consume cow’s milk prior to their first birthday are more at risk of iron deficiency anemia and intestinal distress, which can also contribute to anemia. Why? Cow’s milk is low in iron and babies who drink cow’s milk may reduce their intake of other iron-rich foods.
Can I give baby cow's milk in a bottle?
As a child starts the transition to cow's milk around 12 months old, it might feel like a natural progression to serve milk in baby bottles. We advise against this practice for a few key reasons:
By 12 months of age, most children have become efficient with drinking from a bottle and can rapidly consume several ounces at a time from one. Because they are used to the bottle offering a full meal, serving cow's milk in this way can lead to toddlers taking in too much in one sitting and throughout the day, which increases the risk for iron deficiency anemia and tends to decrease interest in solids.
Unlike formula and breast/human milk during infancy, cow's milk is not meant to be a meal for toddlers. It's a drink to be consumed with a meal at the table. Bottles are often consumed away from the table for both nourishment and comfort, so putting cow's milk in a bottle can create a slippery slope toward a toddler drinking cow's milk throughout the day and away from the table.
Cow's milk in a bottle is associated with increased risk of cavities. The risk is highest when a toddler sips on cow's milk from a bottle throughout the day and when they consume cow's milk at night in bed. These practices can lead to pervasive cavities, commonly referred to as "bottle rot."
Is cow’s milk good or bad for babies?
Compared to breast milk and formula, cow’s milk poses many nutritional disadvantages for babies younger than 12 months of age.
Cow’s milk is low in a number of nutrients but, most importantly, it is low in iron—an essential nutrient that fuels your baby’s brain development. To complicate matters, the type of iron that is present in cow’s milk is not as well absorbed as the form of iron found in breast milk. While cow’s milk has more protein and minerals like calcium and phosphorous, the higher mineral content may increase the risk of dehydration in babies (though evidence is limited). Lastly, early consumption of cow’s milk can take the place of other, more nutritious foods that your baby would have otherwise been eating, increasing the risk of nutritional deficiencies as a result.
Genetics, gut function, and the age at the time of introduction all influence your baby’s response to dairy. Whenever you decide to introduce dairy, be sure to watch for signs that your baby cannot digest dairy (such as stomach pain, gas, and/or diarrhea) and consult your pediatrician for advice.
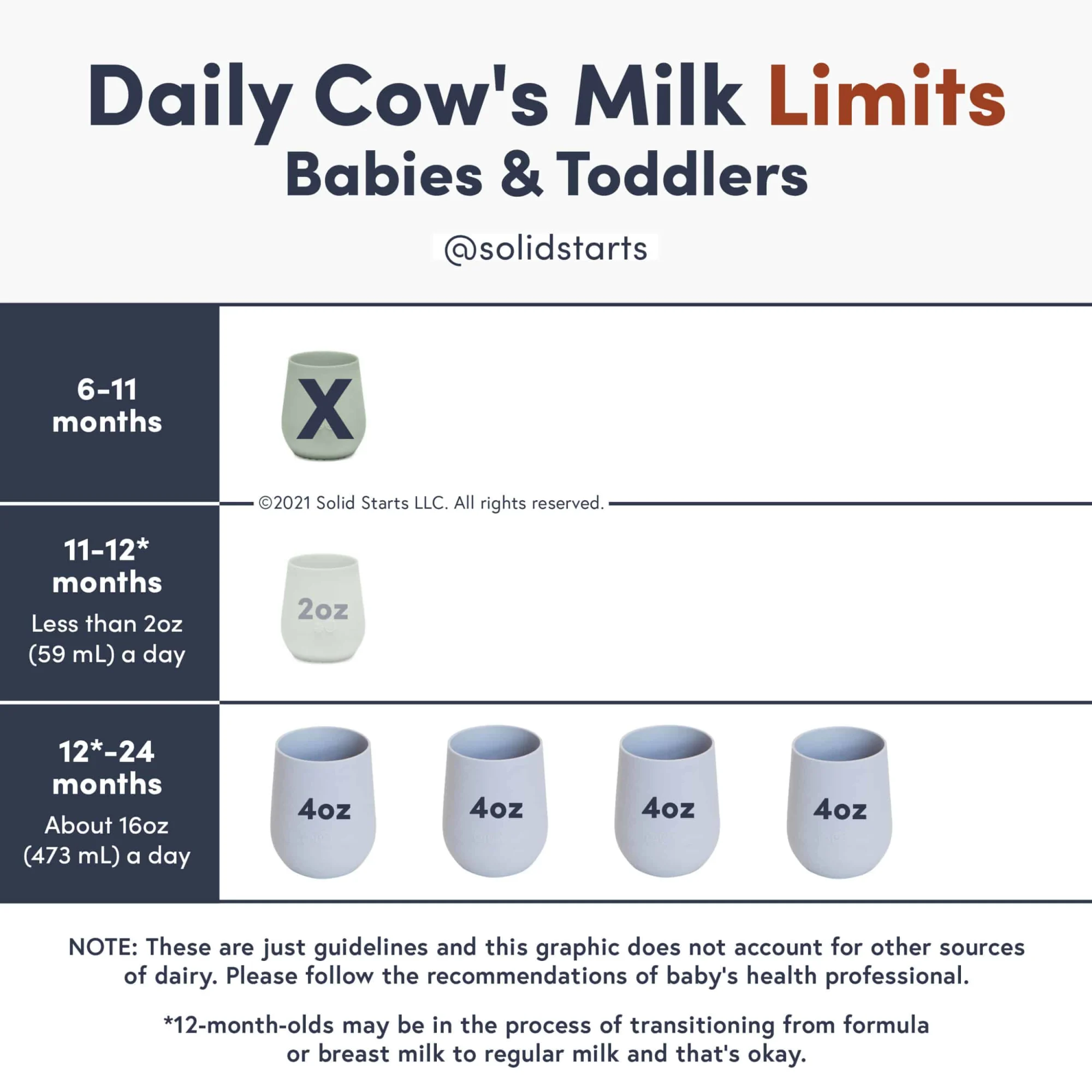
How much cow’s milk can my child drink?
Introduction of cow’s milk is discouraged for babies 6-12 months of age, but it’s fine to offer dairy products such as yogurt or cheese in limited amounts. Around 11 months of age it may be fine to offer small sips of whole cow’s milk (no more than 1-2 oz) in an open cup to practice feeding skills and accustom baby’s palate to the new taste of cow’s milk, as long as it doesn’t displace the intake of breast/human milk, formula, or iron-rich foods. This practice varies across countries, cultures, and health guidance. Beyond 12 months of age, whole cow’s milk is fine to offer to your now toddler, assuming that they have a well-balanced diet that has adequate iron.
Recommendations for dairy intake for 12 months and up are considered in total servings of dairy products in a day, not just from liquid milk alone. This includes servings of yogurt and cheeses, but excludes butter and ghee.
Serving sizes of dairy include the following:
1 cup of milk or yogurt (8oz) = 1 serving of dairy
1-1.5oz of cheese = 1 serving of dairy
1 cup of a calcium-fortified milk substitute like soy or pea protein milk = 1 serving of dairy
Fear not, it’s simpler than it sounds. Let’s break it down by age!
6-12 months: Stick to breast/human milk or formula as baby’s main drink. A little bit of milk mixed into foods is fine as long as it doesn’t replace breast/human milk or formula intake. At this age, there are no set recommendations for total servings of dairy. Aim to limit dairy to 0.5-1 daily servings as baby will be receiving plenty of calcium from breast/human milk or formula and to help prioritize iron-rich foods.
11-12 months: Closer to one year of age and with the go ahead from your doctor, it's okay to offer small sips of whole cow’s milk (no more than 1 to 2 ounces per day) in an open cup to accustom baby's palate to the new taste of cow’s milk. That said, it is also fine to hold off.
1-2 years: Limit milk consumption to no more than 16oz of cow milk per day or 2 servings total of dairy products so milk doesn’t displace valuable nutrients (such as iron) from solids. Opt for whole cow’s milk and whole milk dairy products. If still consuming breast/human milk, the child may not need as many servings of dairy in a day.
2-3 years: Toddlers can have up to 2-2.5 servings of dairy per day. You may hear of recommendations to switch to a lower fat milk, but not all kids need this so be sure to speak with your pediatric health professional for guidance.
Our recommendations slightly vary from the AAP, which recommends 16-24oz of dairy for children 12+ months and is more in line with USDA’s recommendation of up to 2 daily servings of dairy or other calcium-fortified dairy replacements, such as soy or pea protein milk. It is our stance that exceeding 16oz of dairy for 12-24-month-old children risk displacing valuable nutrients (especially iron) from other food sources as it can impede appetite and hunger.
Note: If your child is dairy-free, then these recommendations also apply to milk alternatives like soy and pea protein milks. Cheeses and yogurts made from alternative milks are not usually as nutritious as those made from cow’s milk and are often highly processed. Consider sticking to the dairy-free milk itself as your child’s main source of “dairy,” calcium, and vitamin D.
Does calcium in cow’s milk inhibit iron absorption?
Yes, calcium can affect how our bodies absorb iron from certain foods. Know, however, that your baby’s ability to absorb iron is affected by many factors.
At this stage in life, your baby’s iron levels are already at their lowest and lots of iron is needed for healthy growth. Iron doesn’t affect calcium absorption, but calcium does affect the absorption of iron from plants, meat, and seafood. This is one of the key reasons why cow’s milk is not recommended for babies under 12 months of age. The body is brilliant at self-regulating and studies show that iron status is not necessarily affected by calcium intake because the body will adjust iron absorption when stores are low. Studies also show that the effect of calcium on iron absorption is reduced when a diet consists of a wide range of foods.
For a list of foods that offer the nutrients babies need most, see our Nutrition Cheat Sheet for babies.
What is the best milk for toddlers? Whole milk, low fat, or skim?
The verdict is still out. Whole pasteurized milk is recommended for children under two years of age, at which point many parents are guided to switch their toddler to reduced-fat cow’s milk. However, a summary of 14 studies measuring the effects of consumption of whole milk versus reduced-fat milk shows that higher fat intake correlates with lower weight as children age, and that reduced-fat milk consumption correlates with increased weight or obesity. Whatever fat content you choose, be sure to look for milk without any added flavors or sugars.
Adie, 18 months, asks for more milk.
Hawii, 15 months, downs a cup of milk.
Can cow's milk cause constipation?
Yes. Cow milk, specifically the protein found in cow milk, is notorious for exacerbating constipation. If your child is 12 months and older, we generally recommend trying a non dairy milk alternative such as fortified unsweetened soy or pea protein milk (and we typically advise against toddler formulas unless prescribed by a doctor for weight gain.) Aside from milk, to prevent or ease constipation, make sure your child is drinking plenty of water throughout the day, being offered a varied diet rich in whole foods, and remaining active. Constipation can be a little tricky to treat, so definitely check in with your doctor on the plan of action.
Constipated baby? See our guide How to Relieve Infant Constipation.
Constipated toddler? See our guide 10 Ways to Relieve Constipation in Toddlers.
What about raw milk?
Avoid. Babies’ immune systems are still developing, and raw milk can harbor pathogenic bacteria and other potential contaminants that can increase the risk of foodborne illnesses, which can be fatal to babies. Pasteurization—the process of heating a food to a certain temperature to kill bacteria—is fundamental to reducing the risk of foodborne illness and thus making food safer to eat. For these reasons and more, many medical organizations recommend that all milk for human consumption should be pasteurized.
Can babies be allergic to milk?
Absolutely. Cow’s milk is one of the most common food allergens for babies.
Learn more about common food allergens in our guide Introducing Allergens to Babies.
Can a baby outgrow a milk allergy?
Yes! If your baby is allergic to dairy, be reassured that it is an allergy that often disappears with time. Research shows that the majority of children with cow's milk allergy will outgrow it by age 6 and many babies with milder symptoms of milk protein allergy (which can show up as painless blood in stool) are able to successfully reintroduce cow's milk as early as their first birthday, with the guidance of their doctors.
If baby was diagnosed with CMPA, can they consume other dairy products like yogurt and cheese?
No, unfortunately if baby has CMPA, they can’t have other dairy products, including milk, yogurt, and cheese. Milk from other animals, such as goat and sheep, are also not recommended. Lastly, soy milk or soy-based formula is generally not recommended either, as babies with CMPA can also be sensitive to soy and soy-based products. Remember, research shows that the majority of children with cow's milk allergy will outgrow it by age 6 and many babies with milder symptoms of milk protein allergy (which can show up as painless blood in the stool) are able to successfully reintroduce cow's milk as early as their first birthday, with the guidance of their doctors.
What is the best milk substitute for a baby with CMPA?
If your baby has CMPA, then they should also avoid milk from other animals, as well as soy milk and soy products since babies with CMPA can also be sensitive to these. The good news is that there are a number of other milk substitutes available, such as breast/human milk (from a provider who is avoiding dairy and soy in their diet) or a CMPA-appropriate formula for babies, as recommended by your healthcare provider, or fortified pea protein or oat milk for toddlers. Do note that when compared to cow’s milk, pea protein milk is generally lower in calories and oat milk is generally lower in protein and can be included as part of a generally balanced diet. Be sure to connect with your pediatric healthcare provider such as your dietitian/nutritionist, to help identify the best substitute for your child’s individual needs.
Note: Lactose-free formula or milk would not be appropriate for a child with CMPA. In CMPA, the natural proteins in milk are triggering the allergic reaction. Lactose-free milk still contains these natural proteins but is free of a natural sugar called lactose. Lactose-free milk is appropriate for individuals with lactose intolerance, but keep in mind that lactose intolerance is uncommon in infants and toddlers and is typically not an issue in this age group.
What is the best milk alternative for children sensitive to cow’s milk?
It depends on the age:
0 to 12 months old: Breast milk. Studies show that breast milk is the most tolerated milk for babies.
If you think your baby has sensitivities to infant formulas with dairy, reach out to your pediatrician for guidance. Cow’s milk protein allergy is thought to occur in 2-3% of infants in the US, and approximately 0.5% of breastfed babies. If your baby is formula fed and is having digestive difficulties, they may need to try out hypoallergenic or amino acid-based formulas. For breastfed babies, mom may need go on a dairy-free diet (but consult your pediatrician before self-diagnosing) and ensure she is getting adequate nutrition during this time too. As always, be sure to consult a pediatrician or pediatric gastroenterologist and/or pediatric dietitian or nutritionist when selecting an alternative, as some of these options can still pose a risk for allergic reaction.
12+ months of age: If your baby has a true cow milk protein allergy, they may need to avoid mammalian milks as well (such as buffalo, goat, and sheep milks), in addition to unmodified rice and soy milk as these milks have a risk of also triggering an allergic reaction and may not be nutritionally adequate. However, if your child is sensitive to cow’s milk, but not allergic, they could try alternative mammalian milk, or other plant-based milk alternatives listed below.
What are the best plant-based milks for babies and toddlers?
Not all plant-based milks are created equal when it comes to nutritional value. Furthermore, plant-based milks are considered to be a nutritionally incomplete drink for babies and may promote nutrient deficiencies if they take the place of healthier foods for babies, like breast milk or formula. That’s why general consensus suggests waiting to serve plant-based milks as a drink until after a baby’s first birthday, though cooking foods with plant-based milks for your baby is perfectly fine.
When shopping for plant-based milks, read the labels. You want to select brands of plant-based milks that are fortified with calcium and vitamin D, free of added sugars, low in preservatives, and offer similar protein and calorie content to cow’s milk. Below are our top choices of plant-based milks ranked according to nutritional similarity to cow’s milk:
Soy milk (fortified)
Pea protein milk (fortified)
Oat milk (fortified)
Our guide Best & Worst Plant-Based Foods for Babies explains the nutrients vegetarian and vegan babies need and where to find them.
The chart below shows how popular plant-based milks stack up against mammalian milks, organized by nutritional density across key nutrients babies and toddlers need:
Nutritional content of common animal and plant-based milks
Per 8 oz serving
Milk type | Calories | Fat (gm) | Protein (gm) | Calcium (mg) | Vitamin D (mcg) | Vitamin B12 (mcg) |
Cow | 149 | 7.9 | 7.7 | 276 | 3.2 | 1.1 |
Cow (lactose-free) | 146 | 7.8 | 8 | 300 | 2.7 | 1.3 |
Goat | 168 | 10.1 | 8.7 | 327 | 3.2 | 0.2 |
Sheep | 265 | 17 | 15 | 473 | Unavailable | 1.7 |
Buffalo | 237 | 17 | 9 | 412 | Unavailable | 0.9 |
Camel | 134 | 7.7 | 7.4 | 274 | Unavailable | Unavailable |
Soy | 105 | 3.6 | 6.3 | 300 | 2.7 | 2.1 |
Pea | 70 | 4.5 | 8 | 465 | 6 | 2.5 |
Oat | 160 | 9 | 3 | 350 | 3.6 | 1.2 |
Rice | 113 | 2.3 | 0.7 | 283 | 2.4 | 1.5 |
Almond | 90 | 2.5 | 1 | 451 | 2.5 | 3 |
Coconut | 76 | 5.1 | 0.5 | 459 | 2.4 | 1.5 |
Hemp | 80 | 8 | 2 | 390 | 5 | 0.6 |
Flax | 25 | 2.5 | 0 | 280 | 2.3 | 1.4 |
Macadamia | 50 | 5 | 1 | 585 | 5 | 1.2 |
Breast/human milk | 172 | 10.8 | 2.53 | 79 | 0.25 | 0.123 |
What are the best plant-based milks for toddlers with allergies?
Fortified soymilk or pea protein milk are the most nutritious milk alternatives from the standpoint of nutrients that toddlers need. If your child is allergic to soy or legumes, oat milk is a good alternative. In detail:
Soy, a legume, was one of the first plants to replace dairy. Compared to cow milk, it’s lower in carbohydrates, fats and proteins, and insufficient amounts of calcium and B-12. However, compared to other plant-based beverages, soymilk is one of the best sources of all of these nutrients, and it’s the only plant-based milk with protein levels similar to cow’s milk. Therefore, if your child can tolerate soymilk, that is the most nutritious option. Note that soy contains high levels of isoflavones (which may alter hormones, though no statistically significant data has surfaced), and still poses risk of allergic reaction. For these reasons, soy may not be ideal as the only plant-based beverages offered as a milk alternative.
Pea protein milk, another legume, (often sold under the brand name Ripple), offers fewer carbohydrates and fat than cow’s milk, yet is a great source of protein. It also touts higher levels of calcium, iron and vitamin D than cow’s milk, and is fortified with vitamin B12.
Oat, a pseudo-grain, is low in beneficial fats and proteins, yet has a better amino acid profile that other plant-based beverages. While the fiber in oats may benefit the gut, it’s naturally low in calcium (although it is often fortified with calcium, vitamin D, and vitamin B12) and also contains phytic acid, which may inhibit nutrient absorption.
Also, each of these plant-based beverages has benefits and drawbacks. If using a milk alternative, opt for one that is fortified with key vitamins and minerals (be sure to read labels, as not all are fortified). Some are high on the glycemic index and come in forms that also include added sugars, preservatives, binders and other ingredients that may not benefit health when offered frequently and in large quantities. Lastly, most grains, nuts and legumes grown in conventional agriculture are genetically modified and/or are grown with chemicals. Therefore, consider milk alternatives as a “sometimes” beverage and/or considering rotating the types of milk alternatives you offer.
In most cases, milk alternatives are not recommended to replace cow’s milk (except for health reasons). A well-balanced diet consisting of whole plant and animal foods may offer ideal nutrient intake without cow’s milk or fortified milk alternatives. As always, work with your pediatrician, allergist, and/or pediatric dietitian or nutritionist when selecting a cow milk alternative that is best for your child.
Is almond milk good for babies and toddlers?
Unfortunately, almond milk lacks the protein, fat, and calories we like to see in plant-based milks for toddlers. More nutritious options would be fortified soy, pea, or oat milk---all of which have greater amounts of calories, fat, and protein.
What if my child won’t drink milk?
In general, milk is a great source of protein, fat, carbohydrates, zinc, vitamin B12, and especially, calcium and vitamin D (if the milk if vitamin D-fortified). The good news is that you can find many of these essential nutrients from a wide variety of foods. Let’s hone in on the key nutrients found in milk, calcium and vitamin D. For calcium, you can offer other calcium-rich foods to your child like yogurt and cheese, as well as plant-based sources of calcium like sesame, almonds, broccoli, other dark green vegetables, and tofu or other soy products that are made with calcium. When it comes to vitamin D, there aren’t a ton of foods that are naturally rich in it. Interestingly, yogurt and cheese aren’t usually rich in vitamin D. There is a small handful of vitamin D-rich foods, such as fatty fish, egg yolks, certain mushrooms exposed sunshine/UV-light, liver, and vitamin D-fortified milk alternatives. A note: vitamin D is commonly supplemented, even for those with no dietary restrictions. If your health care provider says your child needs a supplement, don’t worry, low vitamin D levels are common for infants, kids, and adults alike. Bottom line: don’t sweat it if your kid isn’t drinking milk; nutritionally, there are tons of other alternatives to offer.
Amelia, 13 months, refuses cow milk. This is very common with exclusively breastfed toddlers.
How much breast milk can my child drink after their first birthday?
There's no definitive cap on breast milk intake (as there is for cow's milk, for example). However, it’s important to make sure that breast milk isn’t coming at the expense of solid food. After your baby’s first birthday, the primary source of nutrition should be solid food. A good rule of thumb is to limit breastfeeding sessions to 3 to 4 times per 24 hours after your baby’s first birthday and to make sure you are not breastfeeding too close to the solid meals. It can help to think of treating breastfeeds as you would snacks.
For example, make sure you offer solids first, and then if you want to top off with breast milk, wait at least 20 minutes after the solid meal so your child doesn’t hold out for the breast and skip the meal. A breastfeed is about the equivalent of a meal or snack, so if you are breastfeeding on demand and your child isn’t eating well at the table, it's very possible that it’s because too much breast milk is being consumed.
For more information on this topic, check out our video on feeding schedules and weaning.
Is breast milk the same as other milks?
Absolutely not. Breast milk is a very special food, because it is biologically active, meaning it contains unique components that support your baby’s growth, immunity, and gut health. Interestingly, its nutrient composition can also vary depending on a variety of factors, meaning its nutritional content fluctuates. Breast milk, or infant formula, is the ideal source of nutrition for a baby and should be a baby’s sole source of nutrition for the first 6 months of life. From 6-12 months of age, breast milk or formula should continue to be your baby’s primary beverage.
The nutritional composition of breast milk can vary based on a number of factors; some moms may produce fattier breast milk, while others may produce lighter breast milk – no breast milk is the same. What’s more, is that mom’s diet can also impact the nutrients and components found in breast milk, but more research is needed in this area. In general, breast milk may be lower in protein and other nutrients, but higher in fat (to provide plenty of calories to support baby’s growth), when compared to animal and plant-based milks. That said, the nutrients in breast milk are thought to be more available for absorption than other milks. In summary, no other milk, besides infant formula, can replace breast milk for an infant.
How do you properly store breast milk?
The most important thing to keep in mind when storing breast milk is avoiding cross contamination with other foods. All containers for collection and storage of breast milk should be kept clean and sterile.
It is acceptable to store breast milk for up to 4 days in the refrigerator (preferably in the back of the refrigerator to prevent intermittent warming from the door opening). If you are going to freeze breast milk, try to freeze the fresh or refrigerated breast milk within 24 hours as the beneficial enzymes begin to change at approximately 25 hours. This doesn’t have to be a determining factor in the how quickly you freeze your refrigerated milk, but it’s worth consideration.
If not used within 72 hours, fresh breast milk should be transferred to the freezer in a clean, freezer-safe container and dated. While it is acceptable to store breast milk in a deep freezer with an attached refrigerator (0°F or −18°C) for up to 6 months and in a deep freezer (−4°F or −20°C) for up to 9-12 months, the sooner you use it, the better. Frozen breast milk lasts safely in the freezer for one month while preserving most of the nutrients, but after 3 months in the freezer, there is a noteworthy decline in concentrations of fats, calories and other macronutrients.
To thaw, plan ahead and defrost overnight in the refrigerator, and never on the counter. And because heating to excessive temperatures can greatly alter the nutrient quality, refrain from defrosting breast milk in the microwave or on the stove. Once breast milk is completely thawed, you have 24 hours to use it. And remember: breast milk does not have to be heated at all! Many babies will happily drink room temperature—or even cold—breast milk.
Can you cook with breast milk?
Yes, though heat does alter the structure of breast milk. Some studies have suggested that when breast milk is heated to just 100.4°F (38°C)—slightly above body temperature—its proteins begin to break down. This means that even when we heat stored breast milk it can lose important immunologically “active” and digestive components that benefit babies.
While you lose some nutrients in the heating process, cooked breast milk still offers nutritional value, so if you want to cook with your breast milk, go for it. Just know it would be better just to add some fresh breast milk stirred into food after it has been cooked.
Note: If you intend to freeze the food you cook with breast milk, remember to only use fresh breast milk as it is not safe to refreeze breast milk.
My baby has gone on a nursing strike. What do I do?
A nursing strike can usually last a few days to a week, sometimes longer depending on the cause of the strike. Usually, it’s a normal part of infant development, but can also be caused by pain, teething, ear infection. Regardless of the underlying reason, it's stressful! It’s important to note that the baby is not rejecting you or the milk, but just managing a different experience. Milk supply is fairly regulated and a few days of disruption won't drastically impact your milk supply. Additionally, efficient breastfeeding babies will often spend less time extracting enough milk from the breast and expect a reduction in the number of nursing sessions as baby ages and increases solid food intake. Here are some ways to encourage baby back to the breast to continue your breastfeeding journey:
If baby is distracted: nurse in a decreased stimulating environment (like a dark, quiet room), nurse while baby is drowsy or in the baby carrier, try the side lying position, and/or increase the amount of evening/night time nursing opportunities.
If baby is congested or you suspect an ear infection/head cold: nurse in an upright position to help with nasal drainage and use breast compressions as needed to increase milk flow.
Increase skin-to-skin or babywearing. This is particularly helpful if you suspect a pain-related reason for the nursing strike.
If teething: try rubbing the gums with chilled breast/human milk and use teethers that reach back to the molars. Increasing skin-to-skin will also help with this.
Nursing strikes can also happen during pregnancy or menstruation/ovulation. In each of these cases, milk can take on a different flavor and supply naturally decreases.
Can you store formula in the refrigerator?
Yes. Similarly to breast milk, it is important to: avoid cross contamination with other foods, maintain clean surfaces, use sterile containers, keep the refrigerator at less than 41°F or 5°C, and preferably place the formula at the back of the refrigerator to avoid intermittent warming with door openings. If formula is prepared from powder for later use, it should be covered and stored in the refrigerator immediately and is recommended to be used within 24 hours to avoid risk of foodborne illness. If using a ready-to-feed formula, once opened, it can be stored covered in the refrigerator for up to 48 hours. Formula that is left over from feeding your baby should not be stored in the refrigerator and should be thrown away as your baby’s saliva can contribute to the growth of bacteria.
Can you cook with formula?
Yes, though similarly to breast milk, heating formula can also degrade certain nutrients and decrease the bioavailability (the usability) of certain vitamins and minerals.
This can be avoided by adding prepared or powdered formula into foods after cooking. Up to 1 teaspoon of powdered infant formula can be sprinkled onto 4 ounces of soft or puree textured foods. Prepared formula can be used to thin out certain thicker consistency foods and stirred into other foods. That being said, we recognize that feeding your baby can feel overwhelming at times and we want to reassure you that it is completely fine to cook with prepared infant formula as it still provides calories, fat, protein, and other vital nutrients to help your baby thrive.
When can babies drink water?
In small amounts, water may be introduced after 6 months of age. When babies consume water, it puts them at risk of inadequate intake of calories, protein, and essential nutrients. However, per the American Academy of Pediatrics, starting around 6 months of age—and as long as baby is growing and gaining appropriately—small amounts of water can be offered, although not usually required.
While the American Academy of Pediatrics suggests you can offer up to 8 ounces of water per day starting at 6 months old, it is our strong opinion that water should be limited to less than 2 to 4 ounces a day so it doesn’t displace valuable nutrition from breast milk or formula. If you’re concerned about your baby’s hydration status, you can monitor the number of wet diapers and energy levels and contact your pediatrician.
Does my toddler need a toddler formula, transition formula, or another special supplemental drinks?
In short: no. Toddler formulas and “transition formulas” for the most part are not necessary for your child. What’s more, these toddler formulas do not face the same level of regulatory scrutiny as infant formulas. You can continue providing breast milk well into toddlerhood and offer cow’s milk at 12 months of age while focusing on providing a nutritious and diverse diet. Special supplemental drinks, like Pediasure, are not typically required for most toddlers unless there is a medical need. Either way, both of these options tend to have added sugars and preservatives, which are best to avoid where possible. As always, be sure to talk to your pediatric health care provider for more guidance and information on this.
Written by
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
The content offered on SolidStarts.com is for informational purposes only. Solidstarts is not engaged in rendering professional advice, whether medical or otherwise, to individual users or their children or families. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or your medical or health professional, nutritionist, or expert in pediatric feeding and eating. By accessing the content on SolidStarts.com, you acknowledge and agree that you are accepting the responsibility for your child’s health and well-being. In return for providing you with an array of content “baby-led weaning” information, you waive any claims that you or your child may have as a result of utilizing the content on SolidStarts.com.