Sugar in Food for Babies 6 to 12 Months

We are asked all the time: when can babies have dessert and sweet foods? Read on for everything you need to know.
Just starting solids? Be sure to download the Solid Starts App.
At a Glance
Sugar is safe for babies to eat as soon as they are developmentally ready for solid food, which is generally around 6 months of age. However, there can be benefits to waiting.
Wait until 12 months of age to introduce honey due to the risk of infant botulism.
Juice may be offered as a drink in small amounts after 12 months of age, although there are benefits to waiting to serve regularly.
Waiting to regularly offer dessert and food that is high in sugar can help support baby’s interest in exploring a variety of food and flavors.
Regularly consuming juice, dessert, and food that is very high in added sugar can negatively impact oral health and increase the risk of cavities as baby’s teeth erupt.
There is no need to control, track, or restrict sugar, which can create feelings of anxiety and scarcity around food for the whole family that can follow baby as they grow.
There is not an exact amount of sugar that baby can have daily. Aim for a gentle balance: reduce when you can, enjoy when you can’t, and aim to share a variety of food.
Can babies have sugar?
It is safe to offer food with sugar as soon as baby is developmentally ready to start solids, which is generally around 6 months of age, though there are benefits to waiting to regularly serve it.
When can babies have dessert?
Dessert, as long as it does not contain choking hazards (such as candy, large whole seeds, pieces of nuts) or alcohol or caffeine, may be shared as soon as baby is ready to start solids, which is generally around 6 months of age. However, research has demonstrated that regularly offering juice, dessert, and sweet foods can decrease a child’s motivation to try other food. In addition, regularly eating juice, dessert, and other food that is very high in sugar can increase the risk of cavities as baby’s teeth erupt. Aim for balance: allow baby to explore and get comfortable with a variety of foods by offering different colors, flavors, and textures, including sweet foods on occasion. This approach helps teach how sweet food is just one part of what the family eats and enjoys together.
How can I avoid baby developing a sweet tooth?
Babies are born with a preference for sweet flavor, and it is entirely normal for babies to like sweet-tasting food. It is also normal for babies to need lots of exposure to other foods to build appreciation and familiarity with different flavors.
Around 6 months of age, babies are naturally curious and open to exploring all different kinds of food. This developmental window significantly narrows during toddlerhood, which is why we suggest sharing a variety of food as soon as baby is ready to start solids. If you want your child to appreciate different foods and flavors, introduce those foods early on, so that they can get comfortable with them before the natural stage of selectivity arrives in toddlerhood.
The research is clear: the more frequently a food is served, the more likely that food will be accepted and eventually enjoyed by a child. Many foods, such as meats and vegetables, tend to be harder to chew and require more effort to eat than baked goods, dessert, and commercial snacks. Many babies and toddlers are not willing to put in the effort when easier-to-chew food is readily available.
Instead of only sharing food that you think that baby will eat, share meals that you enjoy and let baby explore at the table. Baby looks to you as a role model, and they learn by watching and copying what you do and eat at mealtime. Even if baby simply observes you, or plays with food and ultimately chooses not to eat it, or does not eat very much, the exposure matters. This approach can help motivate baby to explore food that may require more effort to eat.
Bottom line: the goal is not to make baby dislike sweet food, but to show how sweets are one part of a variety of what you eat. It is okay to offer a taste of your dessert and share sweet food that is special to you. We want to model how to navigate a world where sugar is readily available, without shame for enjoying it alongside so many other delicious foods.
How much sugar can babies have each day?
There is no exact amount of sugar that a baby can have each day. Aim for a gentle balance: reduce sugar when you can, enjoy food when you can’t, and aim to share a variety of food.
If you feel an urge to measure, monitor, or track sugar, gently remind yourself that nutrition perfectionism is not the goal, and a taste of sugar won’t hurt. Restricting food and setting strict rules around food can have unintended consequences, including a preoccupation and a strained relationship with sweet food for the whole family, which can follow baby as they grow.
When can I give honey to my baby?
After baby’s first birthday. When babies younger than 12 months consume honey, they are at an increased risk of infant botulism—a rare but potentially fatal condition caused by Clostridium botulinum spores, which can colonize a baby’s gut and produce toxins that attack the nervous system. Children younger than 12 months of age are more at risk because their gut microbiome is still developing. For these reasons, leading health organizations recommend avoiding honey before 1 year of age. See Honey in our First Foods ® Database for more information.
Is it safe to offer sugar water for babies?
Only under direct medical supervision. Sugar water, oral sucrose, or Sweet-ease® are typically offered to very young infants (often newborns) who are undergoing a short medical procedure, such as pricking the heel for a lab test, circumcision, poking a vein for a lab draw, or placing an IV (intravenous line). However, sugar water is one of many non-pharmacological options used to address pain. Others include: skin-to-skin contact, breastfeeding, sucking on a pacifier or bottle, and swaddling. To date, no intervention has been shown to be superior in decreasing pain scores in newborns undergoing heel pricks. If baby is scheduled to undergo a short painful procedure, discuss options with your medical team.
When can baby have juice?
Small amounts of pasteurized juice may be shared as a drink after 12 months of age, although it can be beneficial to wait until the child is older to regularly share juice and other sugary drinks. That said, cooking with juice and an occasional small serving of juice as a drink after the first birthday generally isn’t a cause for concern as part of a varied diet. Check out Juice in the First Foods ® Database for more information.
What about natural sugar in fruit?
Natural sugars in fresh fruit are not a concern for babies or children of any age. Fruit is rich in a variety of nourishing vitamins and minerals, in addition to fluid for hydration and fiber to support regular digestion. Fruit can also be a great way to expose babies to different flavors, such as acidity, astringency, and bitterness. Research supports that eating fruit as one part of a variety of food in the diet leads to increased acceptance of sour flavor, and it is not associated with children preferring sweet food over other food.
However, when it comes to fruit juice, a glass of fruit juice can contain much more fruit per serving than one would consume in its whole form and can lead to the ingestion of a high amount of fruit sugar in one sitting, without the fiber found in whole fruit which helps to regulate blood sugars and digestion, and without the texture that slows a baby down as they attempt to chew. Regularly consuming lots of juice can lead to issues like increased risk of cavities, displacement of other nourishing foods, and diarrhea.
Can babies have stevia and artificial sweeteners?
Avoid sugar substitutes when possible, such as artificial sweeteners like sucralose and saccharin and others like stevia, monk fruit, and more. Overall, information regarding the safety of sugar substitutes for babies is limited. Some research also demonstrates that regularly offering sugar substitutes may negatively impact taste perception, blood sugar regulation, and gut microbiome diversity, though more research is needed.
When can kids have candy?
Hold off on introducing candy until you are confident that your child has both the skill and molars to safely break down candy in the mouth. For some children this may be around 2-3 years of age, others may take longer. Never offer candy to babies, including gummies and soft candies as most candy is a choking hazard due to its texture, shape, or both. Some toddlers may have the skills to eat candy around 24 months of age, while others need more time to practice with hard-to-chew foods. The key is to consider the child’s eating skills, familiarity with firm, slippery food, and ability to follow directions.
How to create a balanced approach to sugar
Be gentle on yourself: reduce sugar when you can, enjoy food when you can’t, and aim to share a variety of food flavors, colors, and textures. There are many benefits to sharing what you like to eat with baby, and sugar in pancake batter, pasta sauce, or stir-fry won’t hurt. The amount of food a baby consumes is typically quite small as they are learning how to bite and chew, and, as a result, the amount of sugar that baby consumes per serving can be quite small. What matters is that baby has exposure to a variety of flavors, colors, and textures to explore as they are learning to eat solid food.
There are an endless number of philosophies on how to navigate sweet foods for baby, and they can get a bit overwhelming. Know that it’s okay to keep it simple and do what works for you. Mealtimes are moments for you and baby to connect and be nourished emotionally and nutritionally.
How can I reduce sugar in baby’s food?
There are various ways to reduce sugar in a baby’s diet:
Avoid sharing sweet drinks like juice or soda
Use less sugar than a recipe suggests
Swap sugar for mashed fruit in baked goods
Look for versions of foods with little to no added sugar, such as plain oats instead of flavored oats, or plain yogurt instead of flavored yogurt
What foods are high in sugar?
Foods that are commonly high in sugar include cake, candy, chocolate, cookies, honey, jam and jelly, marmalade, muffins, sweetened yogurt, and sweetened drinks.
Other foods that are high in sugar include:
Drinks like juice, 100% fruit juice, soda, toddler milks, and flavored milks
Candies like chocolate, gummies, and hard candies
Condiments like barbecue sauce and ketchup
Sweet sauces like caramel and chocolate syrups
Sugars like brown sugar, coconut sugar, granulated sugar, and powdered sugar
Syrups like agave syrup, birch syrup, date nectar, honey, and maple syrup
How does sugar impact a baby’s weight and growth?
Baby’s weight and growth are influenced by many factors and not by food alone. As long as baby is thriving and growing consistently with themselves as their own benchmark, baby is healthy. Focus on creating balance by sharing a variety of food flavors, colors, and textures, and avoid making a big deal of food with sugar. This approach not only nourishes baby with the food they need to thrive, but helps baby develop into a child who feels comfortable in their own skin.
How to deal with negative feelings about sugar?
Start by chasing the “why” behind behaviors and emotions around sugar. For many adults, attitudes toward sugar are shaped by many factors, such as media, beliefs, life experiences, and more. Some worry about baby’s weight, others question the safety of food with sugar, and many fear that baby will struggle with picky eating. Even when one does not experience these emotions, chances are they may encounter sugar stigma from family, friends, and even healthcare providers.
Restricting foods, like those with sugar, can lead to food fixations, eating and appetite struggles, and cycles of shame, guilt, and scarcity, which babies and toddlers learn from the adults and older siblings in their lives. That is why, when sugar triggers big feelings, it is important to try to pause and get curious. Perhaps there is worry that eating sweet food will result in health issues. Acknowledge and accept that it is okay to experience the emotion, then ask, “What is the source of this feeling? Why is the emotion coming now? What are the facts to support it? And what steps can I take to work through them?”
Give yourself permission to do what works for you and your family to have a happy relationship with food. And remember, sugar can be part of a balanced diet when it is consumed among a variety of food.
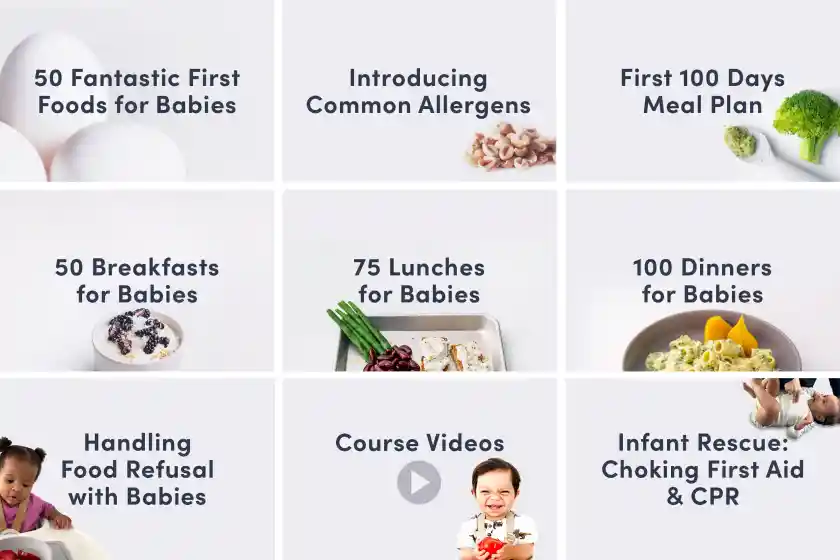
Need more support? Check out our Starting Solids Bundle for babies and our Toddlers at the Table Bundle for children between 12 months and 3 years of age.
Written By
V. Kalami, MNSP, RD, CSP. Board-Certified Pediatric Dietitian and Nutritionist
R. Ruiz, MD, FAAP, CLC. Board-Certified General Pediatrician and Pediatric Gastroenterologist
K. Grenawitzke, OTD, OTR/L, SCFES, IBCLC, CNT. Senior Feeding & Swallowing Specialist
K. Rappaport, OTR/L, MS, SCFES, IBCLC. Senior Feeding & Swallowing Specialist
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
The content offered on SolidStarts.com is for informational purposes only. Solidstarts is not engaged in rendering professional advice, whether medical or otherwise, to individual users or their children or families. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or your medical or health professional, nutritionist, or expert in pediatric feeding and eating. By accessing the content on SolidStarts.com, you acknowledge and agree that you are accepting the responsibility for your child’s health and well-being. In return for providing you with an array of content “baby-led weaning” information, you waive any claims that you or your child may have as a result of utilizing the content on SolidStarts.com.