Infant Formula Shortage FAQs and Guide

While many parents might ask themselves whether or not their baby is consuming enough milk, no one should ever have to worry about where they will get their baby’s next bottle.
This post is intended to provide guidance in a time of severe baby formula shortage. The goal in any health emergency is to keep baby adequately hydrated, nourished, and safe. Keep in mind that the advice provided here is strictly for EMERGENCY situations and does not apply in situations of typical formula access. As always, please talk to your child’s healthcare provider if you have any concerns about your baby’s overall health, nutrition, or growth.
*Note on offering toddler formulas to infants: Make absolutely sure that honey is not listed as an ingredient, given the increased risk of infant botulism.
Navigating the infant formula shortage by age:
0 – 6 Months: Formula and/or breast milk should be baby’s main source of nutrition. If none is available, contact your child’s healthcare provider right away.
Consider reaching out to your local milk bank, as some provide breast milk without a prescription.
Do not dilute formula or breast milk with water or any other liquid.
Do not attempt to make your own formula.
Pediatric store-bought oral rehydration solutions, such as Pedialyte, are acceptable for a couple to a few days under medical supervision.
In an emergency, if baby is at least 4 months old, you may supplement with puréed food and iron-fortified infant cereals so long as it is developmentally appropriate and approved by your child's healthcare provider.
6 – 9 Months: Formula and/or breast milk should be baby’s main source of nutrition. At this age, your baby should be eating solid food too.
If formula or breast milk is unavailable, contact your child's healthcare provider right away.
Do not give water or dilute formula or breast milk with water or any other liquid unless advised to do so by your child’s healthcare provider.
Do not attempt to make your own formula.
Pediatric store-bought oral rehydration solutions, such as Pedialyte, are acceptable for a couple to a few days under medical supervision.
Sips of water are acceptable in limited amounts (no more than 2-4 ounces per day).
As a last resort, if you cannot find any formula, and after consulting with your child’s healthcare provider, for a couple to a few days at a time you may consider offering pasteurized full-fat cow, sheep, or goat milk, fortified non-dairy milk (soy or pea protein are best), and/or toddler formula (make absolutely sure that honey is not listed as an ingredient, given the increased risk of infant botulism).
Depending on your child’s overall diet, they may also benefit from iron supplementation as well, so please discuss this with their healthcare provider.
Focus on offering nutritionally dense solids, such as mashed beans and lentils, meat, poultry, seafood, eggs, thinned out peanut/nut butters, whole fat yogurt, avocado, and oatmeal.
It is fine to continue to offer iron-fortified infant cereals to your baby.
9 – 12 Months: At this age, formula and/or breast milk remain important sources of nutrition with an increasing focus on iron-rich solids.
If formula or breast milk is unavailable, contact your child's healthcare provider right away.
Some water is acceptable (no more than 8 ounces per day).
Do not dilute formula or breast milk with water or any other liquid.
Do not attempt to make your own formula.
Pediatric oral rehydration solutions are acceptable for a couple to a few days at a time under medical supervision.
The vast majority of infants aged 9 months and older can be safely introduced to pasteurized full-fat cow, sheep, or goat milk, and fortified plant-based milks (soy and pea protein are best) for a couple to a few a days at a time, under your child's healthcare provider’s supervision, or longer depending on the individual child and their nutritional needs.
Under medical supervision, toddler formula may be an acceptable option as well. Ensure that honey is not listed in ingredients given the increased risk of infant botulism.
Focus on offering nutritionally dense solids such as meat, poultry, seafood, eggs, thinned out peanut/nut butters, whole fat yogurt, avocado, mashed beans and lentils, and oatmeal.
It is fine to continue to offer iron-fortified infant cereals to your baby.
12 – 24 Months: If your child is eating a well-balanced and varied diet, you do not need to offer infant formula anymore.
At this age, cow’s milk or other ruminant milks provide protein, fat, calcium, and vitamin D, so if you are unable to get milk, focus on foods rich in these nutrients, such as yogurt, kefir, and cheese.
If your access to whole cow’s milk (or other ruminant milk) is limited, consider offering any of these milks: cow, sheep, or goat (2% fat); fortified plant-based milks (ideally pea protein or soy); or toddler formulas (as advised by your pediatric healthcare provider) such as Kate Farms Pediatric, Boost Kids Essentials, or Pediasure.
At 12 months, water should be a regular part of your child’s diet and is unrestricted at this age if your toddler is consuming most of their calories via solid food.
Pediatric oral rehydration solutions are acceptable for a couple to a few days, under medical supervision.
Infant Formula Shortage FAQs:
What do I do if I run out of my baby’s infant formula?
These are exceptionally stressful times. Fortunately, there are a few tips and tricks you can try:
Talk to your child's healthcare provider and/or pediatric dietitian for individualized guidance.
See if your formula type can be switched to a more available brand or version, such as generic brands, a different formula class, or powder or ready-to-feed formulas.
Ask friends or family if they have formula they can spare.
Reach out to formula companies, look at their websites and use the store locator function, call the company and see if they have additional formula or other resources.
Contact your local milk bank to see if donated breast milk is available for purchase.
Try shopping at small shops and drug stores (not just large supermarkets) in case they have more formula in stock.
If available to you, consider buying formula online from a reputable retailer.
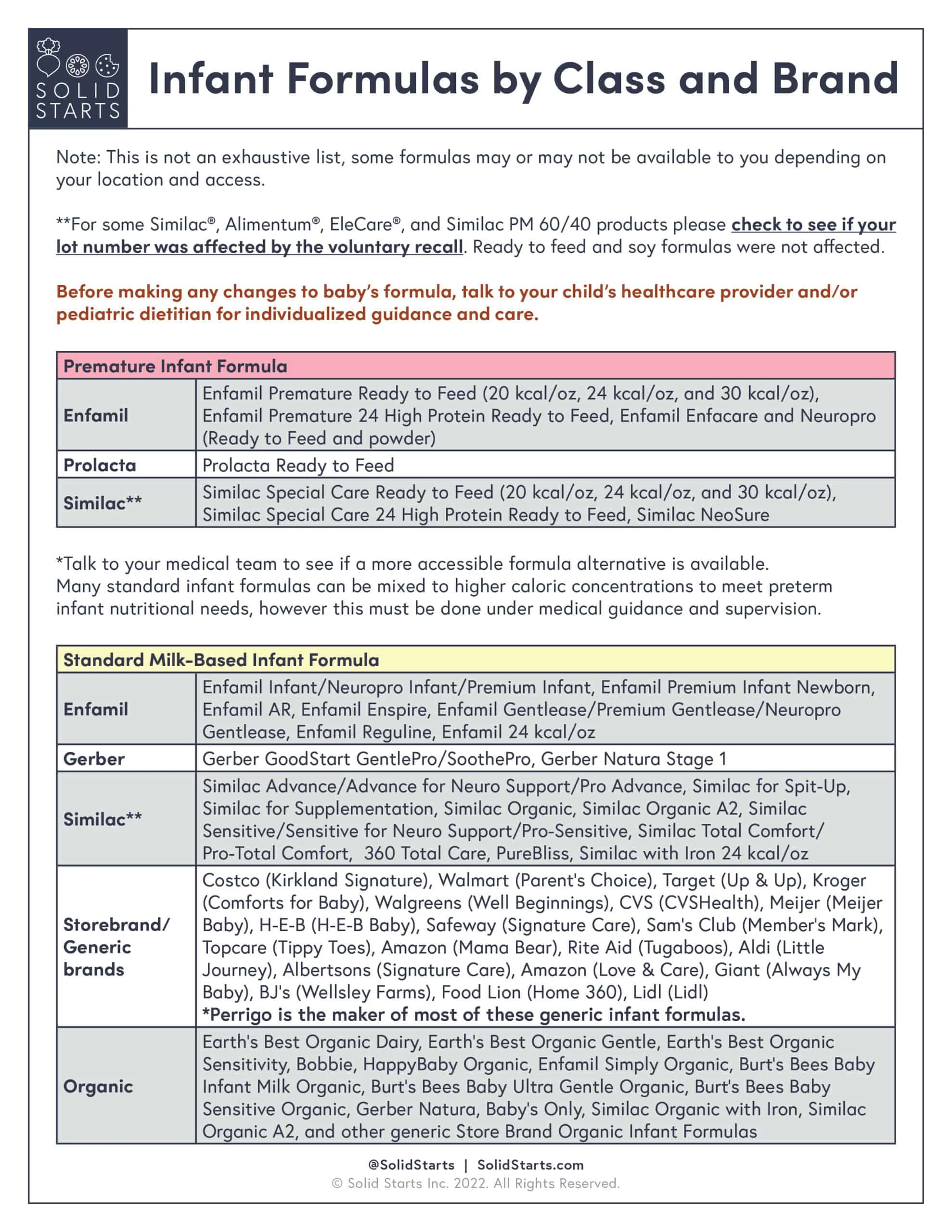
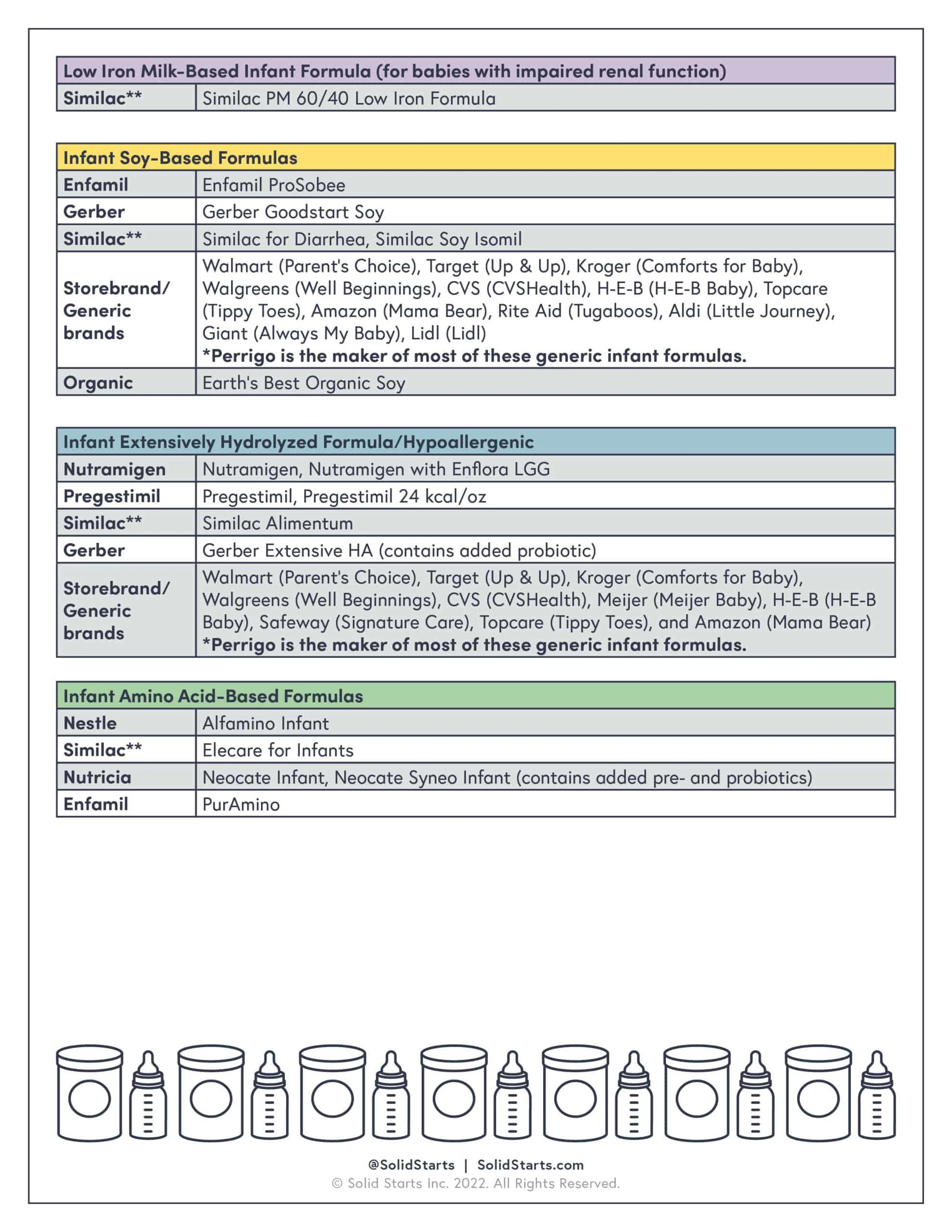
See our table above for a Summary of How to Navigate Infant Formula Shortage By Age and our table below on Infant Formulas by Class and Brand.
The store is out of my baby’s formula, how can I find my baby’s specific formula?
There are a few steps you can take in this situation:
Go to the formula brand’s website and use their store locator function to locate formula near you. If none is available, then talk to your child's healthcare provider and/or pediatric dietitian about the possibility of changing your formula type (if and when appropriate) and/or switching to a generic brand. See our table below for more specific formula information.
Ask if your child's healthcare provider's office or local WIC office (if applicable) has backup formula.
Call the formula company and see if they have a bridge supply they can offer.
Try shopping online through reputable retailers (Target, Buy Buy Baby, Walmart, Costco, Sam’s Club, Instacart, and more) who may have stock of different formulas. You can also try buying directly from the manufacturer's website.
You can also try smaller mom-and-pop stores, your local grocer, pharmacies, etc., and getting to the store as soon as they are open.
Ask your local store when they expect the next formula shipment to arrive and plan to arrive at the store accordingly.
Can I change my baby’s formula to a different kind or brand? My baby requires specialty formula, can they change to another one within the same class?
Generally speaking, yes. However, make sure to talk to your child's healthcare provider and/or pediatric dietitian for individualized guidance. Typically, formulas within a similar class can be used interchangeably; however, you should not switch between different classes of infant formulas unless medically directed to do so. See our table for guidance on alternative options and discuss with your child's medical team.
Can I switch between powder formula and ready-to-feed liquid formula?
Yes, just know that ready-to-feed formulas are significantly more costly. While they are usually recommended for babies 0-2 months, ready-to-feed formulas have similar nutrient composition as powdered formulas.
Is it okay to use generic or store-brand formulas?
Absolutely! All United States infant formulas are strictly regulated by the Food & Drug Administration and must provide essential nutrients a baby needs for optimal growth. Store-brand formulas offer a wide range of formulas depending on your needs. If possible, stay within the same class of formula. If none is available, do not switch formula class before talking to your child’s medical provider or pediatric dietitian. Also, know that, as with any other formula change, it may take your baby’s tummy a couple of days to adjust to a new formula.
Can I dilute my baby’s formula with water to make it last longer?
No. Diluting baby’s formula can lead to dehydration, electrolyte imbalances, kidney problems, weight loss, and even seizures. Infant formula is designed to meet the exact nutritional needs of babies; diluting it may result in the baby not getting essential vitamins and minerals needed for optimal growth and development.
Can I wean my baby off of infant formula? Can I discontinue or change my baby’s formula on my own?
It depends. If baby is close to 12 months of age and has a varied and well-balanced diet that is rich in iron-rich foods, then it may be safe to wean off of formula. However, make sure to first discuss this with your child's healthcare provider and/or pediatric dietitian before doing so. If baby is younger than 11 months, it is not advised to wean off of formula, since it is still providing the majority of baby’s nutritional needs. Discontinuing formula before baby is ready could result in dehydration and growth failure. Before making any changes or discontinuing your baby’s formula, speak to your child's healthcare provider and/or pediatric dietitian for individualized guidance.
The formula my baby needs isn’t available in the right caloric concentration, what do I do? My baby requires a concentrated (higher calorie) formula, what can I do?
Reach out to your child's healthcare provider and/or pediatric dietitian. With very specific guidance, certain formulas can be concentrated or diluted, but this is only done on a case-by-case basis, as needed, and under medical and nutritional supervision. Doing so without proper guidance may result in an overly or inadequately concentrated formula, which could be problematic for your baby’s kidneys, nutrition, and electrolyte balance.
I only see my formula in a higher concentration, can it be diluted to regular concentration (20 kcal/oz)?
Yes, but talk to your child's healthcare provider and/or pediatric dietitian about ways you can safely dilute the formula in order to prevent electrolyte imbalances from excess water intake.
Can I adjust the mixing instructions of my baby’s formula on my own?
No, unless you have been explicitly instructed to do so by your child's healthcare provider and/or pediatric dietitian. Certain formulas can be concentrated or diluted, but this is only done on a case-by-case basis, as needed, and with ongoing medical supervision. Otherwise, continue to follow the mixing instructions on the formula container.
My baby has a feeding tube. Can I still continue to make big, daily batches of formula?
Generally speaking, yes. Just make sure to follow your pediatric dietitian’s instructions for mixing the batches and be mindful to minimize formula waste. When making large batches of formula, such as for tube feedings, it is important to keep the prepared formula that has not yet been used in the refrigerator in order to prevent the growth of harmful bacteria that can cause foodborne illness.
Is it okay to ask for formula from family and friends?
Yes, as long as the formula is the right type, has been properly stored and handled, and is not expired, it should be fine to lean on your family and friends for support with formula during this unprecedented time.
Can I make my own homemade infant formula?
No. Baby formula is painstakingly designed to mimic the nutritional composition of breast milk. Homemade formulas carry significant health risks such as being nutritionally inadequate and being contaminated by harmful bacteria. These homemade formulas can cause fatal health problems such as electrolyte abnormalities, kidney failure, bacterial infections, and more. Under no circumstances should you make homemade formula.
Is it safe to buy baby formula online? Can I buy formula from Facebook Marketplace, Ebay, or Craigslist?
It depends. It is fine if it is purchased from a reputable online seller. However, avoid purchasing formula from unreputable sellers and third-party vendors, such as Ebay, Craigslist, Facebook Marketplace, or others. Buying from unreputable third-party sellers can result in scams, expired formula, and tampering of formula quality. It’s always best to buy from a trusted retailer like a grocery store, pharmacy, or directly from the formula manufacturer.
Is it safe to use my own breast milk that’s been previously frozen?
If the breast milk was properly frozen and thawed, then it is fine to offer previously frozen breast milk. It is acceptable to store breast milk in a deep freezer with an attached refrigerator (0°F or −18°C) for up to 6 months and in a deep freezer (−4°F or −20°C) for up to 9-12 months. The sooner you use it, the better. Frozen breast milk lasts safely in the freezer for one month while preserving most of the nutrients. See our Breast Milk FAQs page for more guidance.
I am still lactating, but my child no longer needs breast milk, should I pump and donate milk? What can I do to help others suffering during the shortage?
If you are able to make a generous donation of breast milk to your local milk bank, it can be a huge help to families in need, as well as to medically vulnerable and hospitalized neonates who depend on donor milk. Call your local milk bank for details on how you can help families in need.
Can I give my 6-month-old baby cow’s milk or other milk alternatives instead of formula?
Only under dire circumstances and when/if advised by your child’s healthcare provider. See our section above on “Navigating the Infant Formula Shortage by Age” for further details.
Should I use European infant formulas during this infant formula shortage?
Generally speaking, as a resident of the United States, it is not advised to use European formulas. However, these are exceptionally extenuating circumstances. If you are choosing to use European formulas as a resident of the United States, use with extreme caution, as European nutritional standards and handling methods can vary greatly. Know that many European formulas are not FDA approved and many have been recalled due to not meeting certain standards. Additionally, news regarding European formula recalls do not always reach residents outside of Europe and can result in consumption of unsafe infant formulas.
The formula container I have is dented, damaged, and/or expired, should I still use it?
No. Do not use any formula that appears dented, damaged, and/or expired, as it may contain harmful bacteria that could cause serious illness for your baby. Furthermore, after its expiration date, nutrients in formula start degrading and bacteria and mold can start growing, which can be dangerous to infants.
How long does formula last? Can I buy in bulk? How much infant formula should I buy at once during the shortage?
According to the Centers for Disease Control, a can of powdered formula that has been opened can last up to a month; however, this can vary from brand to brand. While the use-by or expiration date can be up to one year after it was manufactured, please refrain from buying more than 2-3 weeks' worth in order to allow all families to access the infant formula they require to keep their babies safe.
Since changing my baby’s formula, my baby has had gas, colic, spit up, reflux, and/or changes in pooping, should I stop the formula?
When adjusting formula brands or types, there can be natural adjustments that occur in baby’s digestive system. It can take a few days to a couple of weeks for baby’s digestive system to become accustomed to a new formula. If in doubt, talk to your child's healthcare provider or pediatric dietitian for further guidance. Our page on When to Worry About Baby’s Poop is a helpful resource for further information on baby’s pooping patterns.
Since changing my baby’s formula, my baby hates the taste. What can I do?
When introducing formula for the first time or even changing formulas, it is not uncommon for baby to take some time to adjust to the new formula’s smell and taste. Fortunately, there are a few tips to help baby accept the formula more successfully:
Mix it half-and-half: Before running out of the old formula or breast milk: Prepare both the new and old formula according to the instructions on the can (disregard if using breast milk). Combine either the: 1) old formula and 2) new formula in a 1:1 fashion, or the 1) breast milk and 2) the new formula in a 1:1 fashion. For example, a 4-ounce bottle of milk would consist of 2 ounces of the new formula and 2 ounces of the old formula or breast milk. This approach can help ease baby into the taste of the new formula. Over time, you can increase the proportion of the new formula. It is helpful to work with a pediatric dietitian, if available, for specific guidance on this.
Incorporate the new formula into baby’s foods: Consider stirring in prepared formula (according to the instructions on the can) into foods such as warm cereals, porridges, and other foods. You can even freeze them in popsicle form for a fun, novel, and intriguing food experience (if baby is developmentally ready). Our Popsicles for Babies and Toddlers page offers further guidance.
Keep calm, start small, and try again: Make smaller batches of the new formula to minimize waste. If you have already run out of baby’s original milk, it is okay, know that you have resources and support. When baby shows hunger cues, remain calm, and offer a bottle. If baby rejects the bottle, give baby some time and a break before gently and calmly offering the bottle again. Offering the bottle in a different environment, such as a different room or location, may help with acceptance. Most babies will quickly realize there are no other options and will soon accept the new formula, although full acceptance may take a few days. If baby continues to reject the new formula despite all efforts, please reach out to the child's healthcare provider.
We have access to fresh, unpasteurized cow, goat, or sheep’s milk. Can I give it to my baby?
No. Do not give your baby unpasteurized (raw) milk of any kind. Unpasteurized milk can carry harmful bacteria and other pathogens, like Salmonella, E.coli, Listeria and more. While anyone, regardless of age, can become sick, babies are at higher risk of fatal cases of foodborne illness because of their underdeveloped immune systems.
Can I reheat leftover formula and give it to baby? How can I reduce formula waste and conserve formula?
No, do not save, refrigerate, and reheat leftover formula that has already been offered to your baby. Bacteria from baby’s mouth can contaminate the formula and result in baby getting sick later. Instead, try making smaller batches of formula to reduce waste and conserve formula.
Where can I buy donated breast milk? How can I qualify to buy breast milk? Do I need a prescription to access breast milk?
Contact your local milk bank to see if they have any breast milk for purchase. Ask your child's healthcare provider if baby qualifies for a prescription. Certain milk banks offer breast milk without a prescription.
I use formula to supplement my baby’s intake. Is there any way I can get extra support?
Yes, contact your child's healthcare provider, as they can point you toward a lactation specialist to help support lactation or provide counsel on how to navigate the infant formula shortage. If you receive WIC benefits, call your local WIC Agency for breastfeeding/lactation help and support.
I pump/express breast milk at work, is this a protected right?
Possibly. The federal Break Time for Nursing Mothers law requires all employers covered by the Fair Labor Standards Act (FLSA) to provide accommodations (such as time to pump and a place to pump) for all lactating individuals. If you think your rights to pumping accommodations are being violated, contact a lawyer or legal representative for guidance. Many lawyers in the community offer free consultations.
Further Community Resources (based on HHS)
Community Action Agency (CAA): Your local CAA may be able to provide you with formula or put you in touch with other local agencies that may have different formulas in stock.
Human Milk Banking Association of North America (HMBANA): While some may require a prescription from a medical professional, most HMBANA-accredited milk banks have been distributing donated breast milk to parents in need without a prescription.
United Way’s 2-1-1: You can call to be put in touch with a specialist who may be able to guide you to your nearest food pantry and other resources to locate infant formula.
Feeding America: Local food banks may have infant formula in stock.
Manufacturer hotlines: Some manufacturers, including Gerber, Abbott, and Reckitt, have urgent product request lines (you can ask your child's healthcare provider and/or pediatric dietitian to submit an urgent product request).
The Supplemental Nutrition Assistance Program for Women, Infants & Children (WIC): Some WIC programs have announced that people who receive benefits may be able to purchase different formulas using their WIC benefits due to the Abbott recall. Visit your state’s WIC website to verify if this applies to you.
How can I help support others who are struggling through the formula shortage?
Share this article with family and friends and on your social media channels to help others gain access to more resources.
If you have extra unopened cans or bottles of infant or toddler formula that your child has outgrown, donate it before it expires.
If you are a lactating parent, and you have extra expressed milk, consider milk donation. Contact your local milk bank for more information on how to apply.
Please do not hoard formula and only buy what you need for no more than 2-3 weeks at a time. Please keep others in mind and consider that many families do not have ready access to the latest information, online shopping, and other resources.
Stay vigilant for your friends, social circles, and family with children who rely on formula. What is a shortage in certain areas may not be in others, and you can help keep an eye out during your regular shopping trips.
If your toddler is on infant or toddler formula and is consuming a varied diet and growing well, consider discontinuing unless otherwise advised by your child’s healthcare provider or pediatric dietitian.
Reviewed by:
Dr. R. Ruiz, MD. Board-Certified Pediatrician and Pediatric Gastroenterologist.
V. Kalami, MNSP, RD, CSP. Board-Certified Pediatric Dietitian and Nutritionist.
C. Aycinena Marcos, MS, RD. Registered Dietitian and Public Health/Clinical Nutritionist.
Ready to get started?
Download the app to start your journey.
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
Copyright © 2026 • Solid Starts Inc
