Iron-Rich Foods for Babies

Published: February 20, 2024
Last Updated: February 16, 2026
Iron is important for a baby’s development, and how much iron baby needs depends on their age, diet, and other factors. Our licensed pediatric team explains how babies get iron—and how to spot an iron deficiency.
Need help starting solids? The Solid Starts App can help you navigate first bites and beyond. Start your free trial.
Key Points
✔ Iron is a key nutrient that babies need
It serves countless functions, including brain development and immune function, and this essential nutrient also helps energize the body so it is ready to focus and learn.
✔ Offer iron-rich foods as soon as they are ready to start solids
While they may not eat much at first, babies can still get some iron by licking and sucking foods. The more opportunities they have to explore iron-rich foods, the sooner they learn to eat them.
✔ Iron deficiency is common—and treatable
If a baby shows signs of low iron or anemia, talk with your doctor. Iron supplements are safe, effective, and often necessary—and not a sign you did anything wrong.
Why Babies Need Iron
Around 6 months, the amount of iron stored in a baby’s body from their time in the womb has naturally decreased. While formula and breast milk continue to provide iron for babies, iron-rich foods can also begin to meet baby’s iron needs around this age. They may not consume much as they learn to bite and chew, but with practice and time, regularly offering these foods leads to eating them.
Babies need iron for countless functions, including brain development and immune function, and this essential n
utrient also helps energize the body so it is ready to focus and learn. During the transition to solid foods, formula can meet a baby’s iron needs. While breast milk contains some iron, breastfed babies may need extra support from an iron supplement. That’s okay and not a sign that you did anything wrong. Iron supplements are a safe and effective way of treating iron-deficiency anemia, which is one of the most common nutrient deficiencies worldwide in children under age 5.
High Iron Foods for Baby
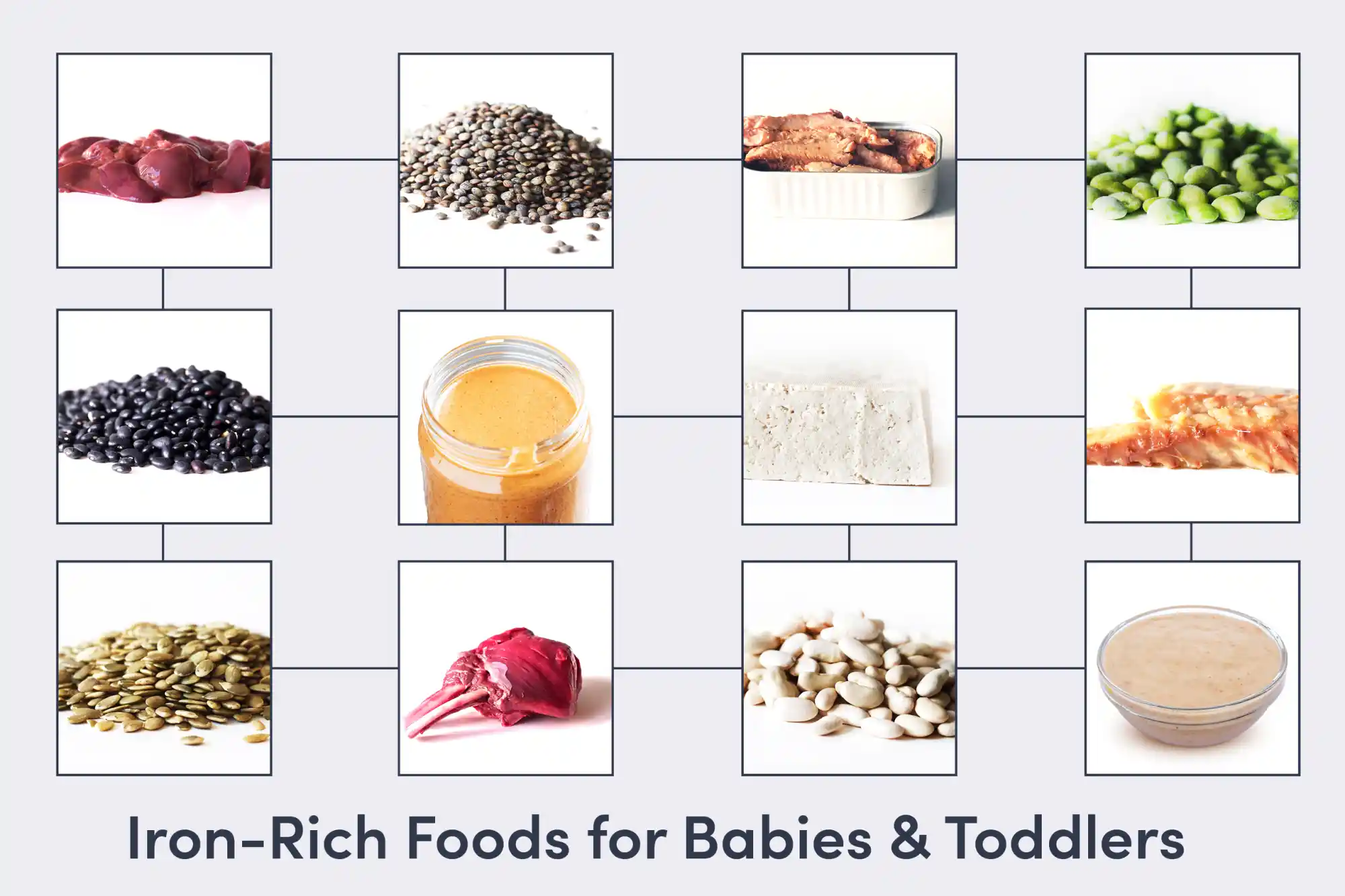
There are two types of iron in foods. Heme iron comes from meat, poultry, and seafood. Nonheme iron comes mainly from plants.
Iron (Heme) | |
Fish | |
Arctic Char | |
Haddock | |
Herring | |
Mackerel | |
Salmon | |
Sardine | |
Trout | |
Poultry | |
Chicken (Dark Meat) | |
Chicken Liver | |
Duck | |
Goose | |
Quail | |
Turkey (Dark Meat) | |
Meat | |
Beef | |
Bison | |
Bone Marrow | |
Buffalo | |
Elk | |
Goat | |
Lamb | |
Mutton | |
Pork | |
Venison |
Iron (Nonheme) | |
Grains | |
Amaranth Seed | |
Fonio | |
Oatmeal | |
Millet | |
Quinoa | |
Semolina | |
Spelt | |
Teff | |
Wheat | |
Legumes | |
Beans | |
Chickpea | |
Edamame | |
Kidney Bean | |
Lentils | |
Peas | |
Peanut Butter | |
Tempeh | |
Tofu | |
Nuts & Seeds | |
Almond Butter | |
Cashew Butter | |
Chia seed | |
Hemp Seed | |
Pumpkin Seed Butter | |
Sesame Tahini | |
Sunflower Seed Butter | |
Vegetables |
|
Amaranth Leaves | |
Beet Greens | |
Collard Greens | |
Spinach | |
Sunchoke (Jerusalem Artichoke) | |
Swiss Chard | |
Egg | |
Chicken Egg | |
Duck Egg | |
Quail Egg |
Vitamin C and Iron-Rich Plant-Based Foods

The body absorbs heme iron more easily than nonheme iron. If you do not eat meat, poultry, or fish, pair iron-rich plants with foods that are high in vitamin C to help the body absorb more of this key nutrient.
Iron-Rich Food | Vitamin C Pairing |
Oatmeal | Blueberry |
Beans | Tomato |
Lentils | Bell Pepper |
Peas | Potato |
Peanut Butter | Strawberry |
Tofu | Broccoli |
Signs of Iron-Deficiency Anemia in Babies
Iron-deficiency anemia is a blood disorder. A baby with iron deficiency or iron deficiency anemia may consistently experience one or more of the following symptoms:
Pale complexion
Poor sleep
Irritability
Difficulty engaging in activities
Challenges with feeding
Decreased appetite
Fatigue
Iron-deficiency anemia occurs when an individual does not have enough iron in the body for a prolonged period of time to produce red blood cells properly, which distribute oxygen throughout the body. Over time iron deficiency can progress into iron deficiency anemia, when red blood cells don’t function optimally and can negatively impact brain development, mood, learning, and growth and development.
In many cases, symptoms of iron deficiency or iron deficiency anemia can take a few weeks to a few months to appear, although this varies. If baby is consistently experiencing these symptoms, reach out to your pediatrician right away. To help identify low iron levels, the American Academy of Pediatrics recommends that babies receive routine screening for anemia around 12 months of age. If your doctor doesn’t mention an iron screening, it is perfectly appropriate to ask about it.
How to Boost Iron in Baby’s Diet
There are many ways to help baby get more iron in the diet as they learn how to eat solid foods. A good way to start is to regularly offer a variety of iron-rich foods. You can also try out these tips.
How to Boost Iron in Baby's Diet | |
Fortified foods | Many foods have iron added to them, such as bread, pasta, and infant cereals. |
Vitamin C & iron-rich food | Pair foods rich in vitamin C with plants rich in iron to help the body absorb more of it. |
Nut and seed butters | Stir into porridge, batter, and sauce. |
Finely ground-up nuts & seeds | Mix into mashed vegetables or batters, coat slippery fruit, or sprinkle on porridge or yogurt. |
Batch cooking | Cook a big batch of beans or meat, then freeze for future easy grab-and-go meals that are iron-rich. |
Cast-iron pan | Cook food in a cast-iron pan to add iron (nonheme) to it. The longer it cooks, the more iron it contains. |
Combine plant and animal sources | Proteins in meat help the body absorb more iron from plant-based foods that are rich in iron. |
Iron-Rich Meal Ideas for Baby
Blend canned beans with oil or yogurt and your favorite seasonings to make a dip.
Try pasta made from chickpeas, lentils, or other legumes.
Use nut or seed flour or iron-fortified wheat flour to make pancakes.
Make a big batch of meatballs or sauce made with beef, lamb, or another red meat.
Mix seed or nut butter with water to make a sauce for noodles, tofu, or vegetables.
Frequently Asked Questions
How much iron do babies need?
The recommended daily intake of iron is 11 mg for babies between 7 and 11 months of age in the United States. Most babies do not consume this much, and yet they are able to maintain a healthy storage of iron in the body. How is this possible? Because the recommendation is inflated. It assumes iron in solid food is coming from fortified infant rice cereal, which is harder to absorb than iron from meat and other animal sources.
Try to let go of the urge to count milligrams and focus on regularly offering iron-rich foods so baby can gradually build the skills to eat them. Formula can meet their iron needs for now, and while breast milk contains some iron, some breastfed babies may need a little extra support from an iron supplement. This is not always necessary, so talk to your pediatrician or dietitian for guidance.
How to get 11 mg of iron with baby-led weaning?
Most babies do not consume this much, and yet they are able to maintain a healthy storage of iron in the body. Focus on regularly offering iron-rich foods and trust that, with practice and time, baby will build the skills to eat the foods that they need to get plenty of iron at mealtimes. When families regularly offer iron-rich solid foods, most babies are able to meet their iron needs over time. In addition, iron-fortified formula meets a baby’s iron needs during this transition; for breastfed babies, talk to your doctor to explore if an iron supplement is necessary.
What if my baby doesn’t eat much iron-rich foods?
Try to be patient and focus on offering a variety of iron-rich foods in a calm and pressure-free environment. Regular exposure eventually leads to eating, and as they are learning, exploring and playing with iron-rich foods can help get some iron in the belly. For example, babies can get some iron by munching on a meatball or licking fingers dipped in bean puree. It can also help to gently remind yourself that breast milk and formula typically provide plenty of nourishment until baby has the skills to eat a variety of solid food. If you are concerned, talk to your pediatrician for guidance and ask if an iron supplement is needed.
Does dairy impact iron absorption?
Not in the long-term when a variety of food is consumed. In the very short term, calcium in dairy products can block some of the absorption of iron, but this is expected and okay as long as baby consumes a variety of food over time. However, regularly consuming excessive amounts of dairy products may result in lower consumption of food containing iron, thereby reducing iron absorption and increasing the risk of iron deficiency anemia.
Do babies need infant rice cereal for iron?
Not necessarily, but some families may choose to offer it. Most babies on formula get plenty of iron, and most babies (including breastfed babies) can get iron from solid foods as soon as they are ready to start eating it around 6 months of age. If you would like to offer infant cereals, consider an iron-fortified oat or multigrain cereal. Infant cereals made with oats, wheat, or a combination of grains can help reduce the risk of accidental exposure to heavy metals like arsenic in rice cereal.
What are iron supplements for babies?
Talk to your pediatrician. Every child has different needs, and your pediatrician can help you determine the type and amount of iron supplement that is appropriate to help avoid excess iron in the body, digestive discomfort, and other issues that can arise with iron supplements. Iron supplements for babies usually come in the form of liquid drops that can be given on its own via an oral syringe for best absorption. If baby doesn’t like the taste, it can also be mixed with breast milk or formula, but iron absorption may be reduced.
Many babies need iron supplements, and if your doctor recommends iron supplements, know that it is normal and you did not do anything wrong. The body's iron stores and ability to absorb iron is impacted by factors beyond diet alone (if baby was premature, for example) and iron supplements are a safe and acceptable solution until baby’s iron levels are restored and the child has the skills to get enough iron from eating solid food.
What if my baby has low iron even after doing everything right?
You are not alone. Every baby is different, and sometimes the body just needs a little extra support, and that’s okay. Know that you have done your very best, and your doctor can help you find a treatment plan that best supports you and your child.
Written By
V. Kalami, MNSP, RD, CSP. Pediatric Dietitian/Nutritionist.
M. Suarez, MS, OTR/L, SWC, CLEC. Pediatric Feeding/Swallowing Specialist.
K. Grenawitzke, OTD, OTR/L, SCFES, IBCLC. Pediatric Feeding/Swallowing Specialist.
R. Ruiz, MD, FAAP, CLC. Pediatric Gastroenterologist.
Ready to get started?
Download the app to start your journey.
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
Copyright © 2026 • Solid Starts Inc
