Getting Started with Allergens
You are about to begin introducing common allergens to your baby. Allergists and medical institutions recommend introducing common food allergens early, and keeping them in your baby’s diet consistently to prevent the development of food allergies.
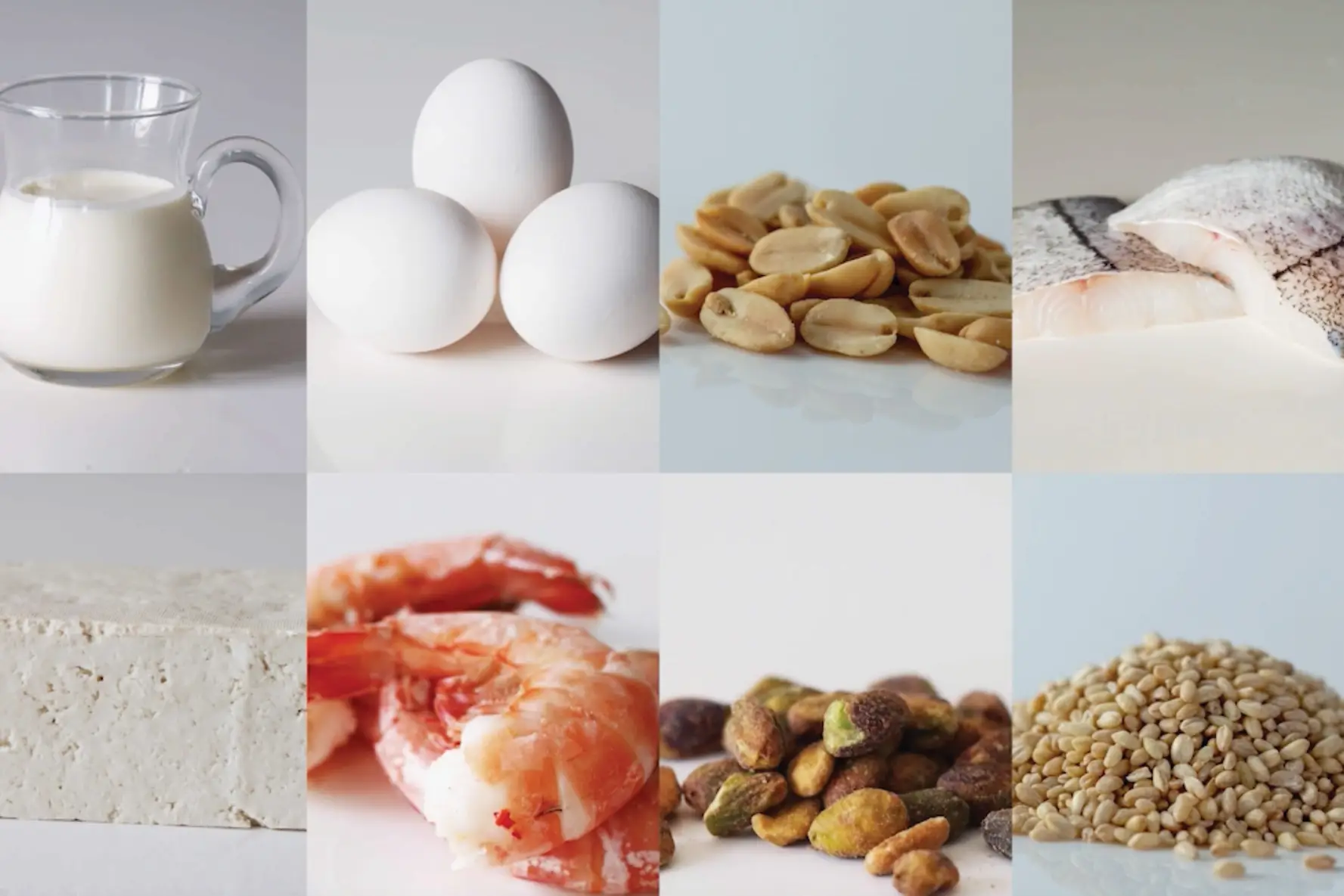
The most common food allergens are: cow’s milk, egg, finned fish, shellfish, peanut, tree nut, sesame, soy, and wheat. This module will walk you through introducing egg, peanut, and cow’s milk: the three allergens with the strongest evidence to support early introduction, and then will give you ideas to keep them in your baby’s diet.
Sakina Bajowala, MD answers frequently asked questions about allergen introduction.
Getting Started
While many caregivers feel anxious about introducing allergens, the research tells us that only 3% of babies will develop a food allergy during the first year of life. As the protective benefits of early introduction are significant, it is important to begin introducing allergens as soon as baby is developmentally ready to begin solids. For most babies, there is no reason to delay home-based introduction beyond ~6 months of age or wait for allergy testing prior to introduction. Although only babies with a personal history of allergy require a prescription for epinephrine (adrenaline), keeping a long-acting, non-sedating antihistamine such as cetirizine (Zyrtec) or levocetirizine (Xyzal) on hand can be useful in the unlikely event of mild allergy symptoms.
Consider Baby’s Risk Factors
There are two main risk factors that indicate your baby might be at an increased risk of developing food allergies: moderate or severe eczema and existing food allergies. If your baby has either of the above risk factors, talk to your child’s medical provider before introducing allergens to come up with a plan.
How You Do it
Avoid sick days: Introduce a potentially allergenic food on a day that baby is overall healthy. This way, you can pinpoint any symptoms of an allergic reaction to food rather than sickness.
Start small. The smaller the quantity served, the less severe an allergic reaction may be. If there is no reaction, gradually increase the amount over the next few days. Once you’ve ruled out an allergy to that food (a few days of daily ingestion is enough to establish that a food is well tolerated), aim to offer it to your baby at least once a week.
Introduce allergens early in the day if possible. Most allergic reactions occur within two hours of ingestion and often within minutes. Introduce allergens in the morning or right after a morning nap so you can observe your child during the day ahead; should an allergic reaction occur, it is easier to contact your doctor for guidance.
Introduce one food allergen at a time. This way, if there is a reaction, you’ll know which food was responsible. Don’t be afraid to offer multiple new foods each week, as long as you aren’t introducing common food allergens simultaneously–don’t introduce two new allergens on the same day.
Don’t worry too much about volume: if your baby doesn’t consume the entire serving of allergen offered that day, that’s ok. Relatively modest quantities of allergen exposure (~2 grams of protein per week) can be effective for allergy prevention, as long as exposure remains consistent.
Regular exposure. Once you’ve safely introduced a food allergen to your child, keep that food in regular rotation—consistency is key. Allergists often recommend aiming for the inclusion of common allergens 2-3 times per week but don’t stress if you can’t get each common allergen on the menu that frequently.
How do I introduce food to baby if I am allergic to it?
Rest assured that you are unlikely to experience a serious allergic reaction from simply being in the vicinity of the allergen or even from handling it. Most patients with food allergies react only upon ingestion. That said, there are ways to minimize your risk.
When preparing the food, avoid prolonged skin contact with the allergen.If you cannot wash your hands promptly afterward, wear gloves.
If you have a carpet or rug, place baby’s high chair over a splat mat or move the high chair to a non-carpeted surface or even consider feeding baby outside. This is also a great time for disposable placemats, plates, and utensils.
When introducing the allergen, offer it at the beginning of the meal and immediately follow up with another food to which neither you nor baby are allergic. This reduces the allergen content in baby’s saliva.
After mealtime, clean baby’s hands and face thoroughly, wipe down the eating surface and chair, and remove baby’s clothing so it can be washed.
It is important to model a calm demeanor, even if you are nervous at first. Children absorb anxiety of the adults around them. As feedings continue successfully, they will get easier and become routine. If you feel very nervous, this is an excellent opportunity for a non-allergic parent, caregiver, relative, or friend to spend quality time with baby.
What do allergic reactions look like?
Allergic reactions often occur within minutes of consuming the allergenic food. There is, however, a small percentage of babies who may experience a delayed allergic reaction, typically presenting as GI symptoms. Your baby may not have an allergic reaction the first time they are exposed to the food, so be watchful on the second and subsequent exposures.
Mild symptoms of an allergic reaction can include ONE of the following
Itchy or runny nose, sneezing
Itchy mouth
A few isolated hives, mild itching
Mild nausea or gastrointestinal discomfort
If you note any of these symptoms, stop feeding the allergen and contact your health care provider for guidance.
More severe reactions may include any of the following, either alone or in combination:
Shortness of breath, wheezing, repetitive cough
Pale, ashen or bluish skin
Swelling of face, lips, or tongue
Widespread hives on body
Repetitive vomiting
Sudden tiredness/lethargy/seeming limp
If your child is having any of the above symptoms or multiple mild symptoms, call 9-1-1/local emergency services immediately and request an ambulance with autoinjectable epinephrine. Do not wait.
What if my baby is allergic to a food?
At any point in the plan, you may substitute ingredients to meet the circumstances of your child. You can, simply swap the allergenic food for a suitable substitute. Here are some common substitutions:
Cow’s Milk. Try a plant-based alternative like soy milk or pea milk once soy and/or pea have been safely introduced. Soy milk is often fortified with iron—an added bonus. Once tree nuts have been safely introduced, you can use a milk made of these common food allergens.
Yogurt. Consider a plant-based alternative like coconut yogurt. After soy and tree nuts are safely introduced, you can use a yogurt made of these common food allergens.
Egg. Eggs are the trickiest ingredient to substitute because they serve multiple purposes. Check out our egg substitution ideas and use a substitute that is appropriate for the recipe you’re preparing.
Peanut and Tree Nuts. For babies with peanut allergy, or an allergy to a specific tree nut, opt for sunflower seeds or sunflower seed butter. Alternatively, try another finely ground-up tree nut or an unsweetened (honey-free) nut butter after that tree nut is ruled out as an allergen.
Finned Fish. For the purpose of this plan, try substituting freshly flaked fish with ground meat or beans.
Soy. Instead of tofu, use beans, ground meat, or a dairy-product like fresh mozzarella cheese, ricotta cheese, or yogurt. For recipes that call for edamame, use garden peas or bean of your choice.
Wheat. Like egg, the best wheat substitute depends on the recipe. Swap coconut flakes when a recipe calls for rolling slippery foods in breadcrumbs. Try lentil pasta instead of wheat pasta. Opt for corn tortilla or another wheat-free bread when bread is on the menu.
Ready to get started?
Download the app to start your journey.
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
