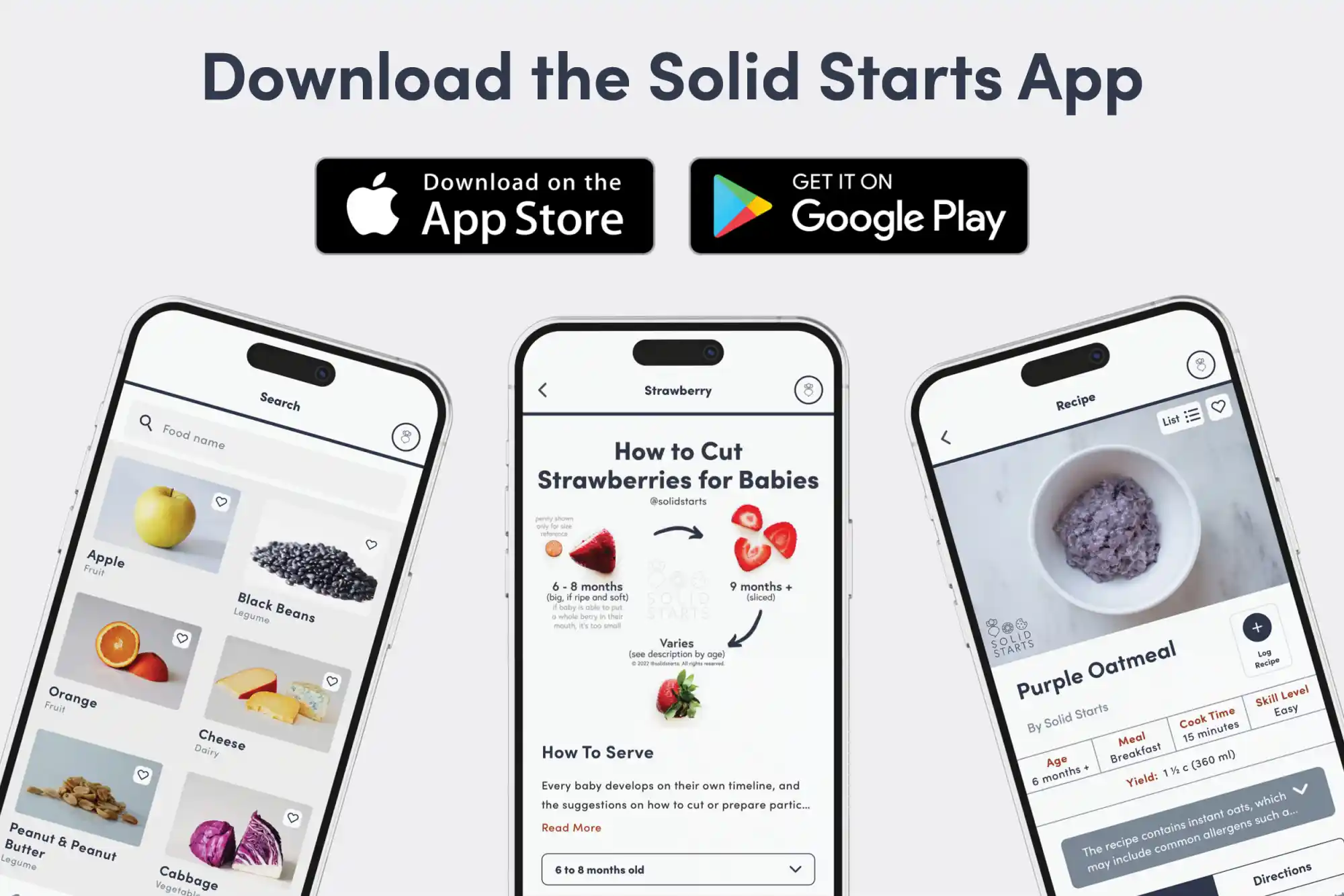
Access our First Foods® Database in the Solid Starts App.
Learn moreBlue Cheese
Dairy
Age Suggestion
12 months
Iron-Rich
No
Common Allergen
Yes

Warning
Mold-ripened cheeses, like blue cheese, carry an increased risk of foodborne illness, such as Listeria, and babies are more at risk for severe symptoms. Raw milk cheeses, like unpasteurized blue cheese, carry the risk of several infections, some of which can be serious and even fatal. There is no age at which it is considered completely safe to offer raw/unpasteurized cheeses to babies and children.
When can babies have blue cheese?
Consider waiting until a child is at least 12 months of age before introducing pasteurized blue cheese due to the increased risk of foodborne illness. Note that baking pasteurized blue cheese to an internal temperature of at least 165 degrees Fahrenheit (74 degrees Celsius) significantly reduces the risk of foodborne illness. All babies and young children should avoid consumption of unpasteurized blue cheese.
Blue cheese is the common name for a sprawling family of cheeses that are made by introducing edible molds into the milk of cattle, goats, or sheep as it ferments to make cheese. Because there are many kinds of blue cheese, there are also many regions that have their own style, from Dorset Blue Vinny in the United Kingdom, to Roquefort in France, to queso de cabrales from Spain. The flavor of blue cheese varies widely as well, from creamy to rich and salty to tangy.
How do you serve blue cheese to babies?
Every baby develops on their own timeline, and the suggestions on how to cut or prepare particular foods are generalizations for a broad audience.
6 to 11 months old:
Consider waiting due to the risk of foodborne illness. Opt for other pasteurized cheeses such as emmental, goat cheese, mascarpone, fresh mozzarella, ricotta, paneer, labneh, or swiss cheese.
12 months old +:
After baby’s first birthday, you can consider offering pasteurized blue cheese, if desired. Consider the risk factors of the child (current health, age) and the source and handling of the cheese. When you are ready to introduce it, you can offer thin slices or bite-sized crumbles of pasteurized blue cheese. To further reduce the risk of foodborne illness, pasteurized blue cheese can be baked to an internal temperature of at least 165 degrees Fahrenheit (74 degrees Celsius). Make sure there are no large firm globs of melted cheese in the child’s portion of the meal, as these pose an increased choking risk. Avoid unpasteurized blue cheese.


Videos
Is blue cheese a choking hazard for babies?
Yes. Cheeses like blue cheese are firm and can get globby and hard to manage in the mouth, qualities that increase the risk of choking. To reduce the risk, prepare and serve blue cheese in an age-appropriate way as described in the How to Serve section. As always, make sure you create a safe eating environment and stay within an arm’s reach of baby during meals.
Learn the signs of choking and gagging and more about choking first aid in our free guides, Infant Rescue and Toddler Rescue.
Is blue cheese a common allergen?
Yes. Blue cheese is commonly made from cow’s milk which is a common food allergen in young children, with dairy accounting for about one-fifth of all childhood food allergies in the United States. Blue cheese can also be made with goat’s and sheep’s milk. Keep in mind that dairy products from ruminants such as sheep, goat, and buffalo may provoke similar allergic reactions to cow’s milk dairy products. If baby is allergic to dairy, know that it is an allergy that often disappears with time. Research shows that the majority of children with cow's milk allergy will outgrow it by age 6, and many babies with milder symptoms of milk protein allergy (which can show up as painless blood in stool) are able to successfully reintroduce cow's milk as early as their first birthday, with the guidance of their doctors. Note: Aged cheeses generally contain histamines, which may cause rashes in children who are sensitive to them.
Milk is a known cause of food protein-induced enterocolitis syndrome, also known as FPIES. FPIES is a delayed allergy to food protein which causes the sudden onset of repetitive vomiting and diarrhea to begin a few hours after ingestion. Left untreated, the reaction can result in significant dehydration. Thankfully, like other forms of milk allergy, FPIES that presents early in life is generally outgrown by the time the child has reached 3 to 5 years of age. While the exact rates of FPIES are unknown, it is believed to be an uncommon condition (although better recognition of the disease has led to increased reporting in recent years).
For those with older children who are lactose intolerant (keep in mind this is uncommon for babies and toddlers), some good news: compared with milk and certain other dairy products, many cheeses may be better tolerated by those with lactose intolerance, particularly aged cheeses, which have lower lactose content. Note that if a child is lactose-intolerant, it’s important to find calcium-rich foods to consume regularly to ensure a balanced diet and support bone health. Search for naturally low-lactose cheeses and dairy products labeled “lactose-free.”
If you suspect a child may be allergic to dairy products, consult an allergist before introducing other dairy products like cheese. Based on baby’s risk factors and history, your allergist may recommend allergy testing, or may instead advise dairy introduction under medical supervision in the office. If the risk is low, you may be advised to go ahead and introduce cheese in the home setting. As with all common allergens, start by serving a small quantity for the first few servings, and if there is no adverse reaction, gradually increase the quantity over future meals.
Is blue cheese safe for babies?
It depends. It can be, if pasteurized and baked to an internal temperature of at least 165 degrees Fahrenheit (74 degrees Celsius), but waiting until a child is at least 12 months of age can further decrease the risk of illness. Unpasteurized blue cheese of any kind, on the other hand, carries a significantly increased risk of foodborne illness at any age.
Does baby need a high chair?
While a high chair can help create a safe eating environment, there are alternative ways for baby to eat safely, such as holding the child on your lap or sitting together on the floor. For more information, see our article on high chairs.
What utensils do I need to get started?
None! Put solid food directly on baby’s tray, plate, or bowl, then let baby explore with their hands. If you like, keep a baby spoon or fork nearby to help familiarize the child with utensils, but the skills to use them are not expected until early toddlerhood.
Our Team
Written by
Expert Tips Delivered to Your Inbox
Sign up for weekly tips, recipes and more!
Copyright © 2026 • Solid Starts Inc